In this section, we describe the key features of the Bedside Learning Coordinator (BLC) role and how it aligns with a learning health system approach.
The Bedside Learning Coordinator (BLC) role was created at the NHS Nightingale Hospital London during the first wave of the COVID-19 pandemic. The BLC role was designed to support the wider learning health system (LHS), capturing staff insights into what was and was not working, and rapidly feeding these insights back to the leadership teams to review and agree how to respond, implementing required actions as appropriate.
NHS trusts across England are now adopting the BLC role across different settings, turning this from a pandemic response to business as usual, allowing them to capture insights on improving patient care, efficiency and staff wellbeing.
What is the BLC role?
How the BLC role works
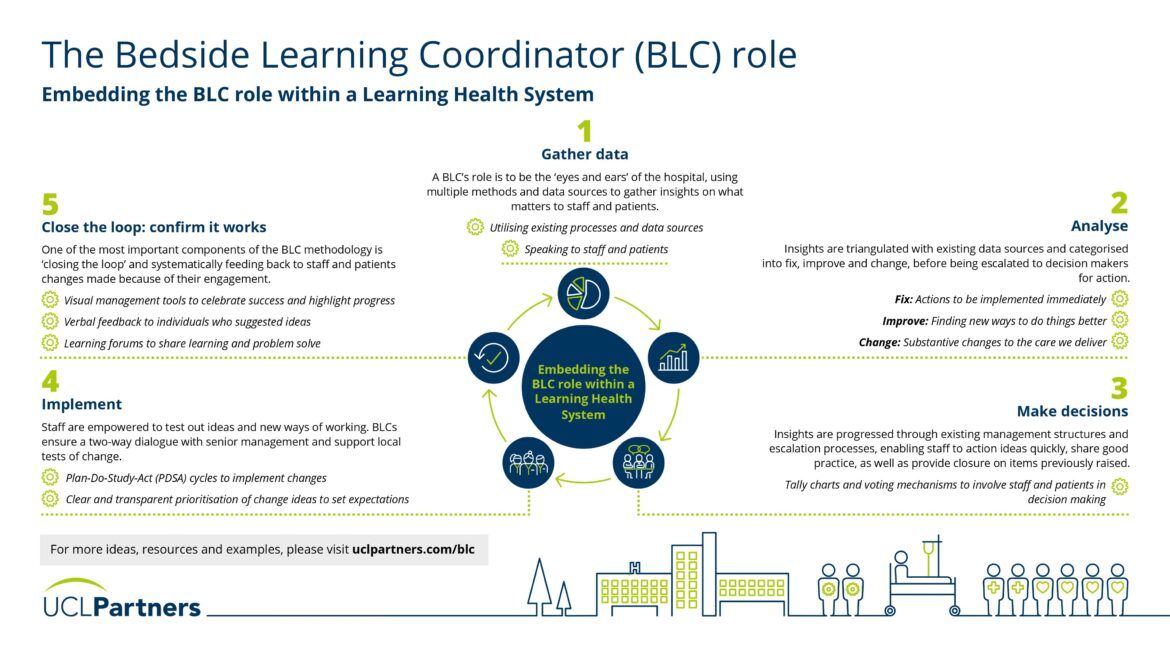
Embedding the BLC role within a Learning Health System
Learning Health Systems help organisations to learn and act fast to drive improvement. The BLC role is not a standalone intervention, it is designed to be embedded in a wider learning health system. It is critical to ensure insights are triangulated with other data sources and rapidly fedback to decision makers to review and implement changes.
Step 1: Gather data
A BLC’s role is to be the ‘eyes and ears’ of the organisation, using multiple methods and data sources to gather insights on what matters to staff and patients. In practical terms, this may include speaking directly to staff and patients in clinical and non-clinical areas, reviewing existing data sources e.g., staff surveys or gathering insights from huddles and team meetings.
Step 2: Analyse
Insights are triangulated with existing data sources and categorised into fix (actions that can be implemented quickly and easily), improve (new ways of doing things better) and change (substantive changes requiring further input), before being escalated to decision makers for review and action.
Step 3: Make decisions
Insights are progressed through existing management structures and escalation processes, enabling staff to action ideas quickly, share good practice, as well as provide closure on items previously raised. The aim of this process is to complement existing governance structures rather than overriding them or ‘reinventing the wheel’. Staff and patients can also be involved in decision making through tally charts and other voting mechanisms.
Step 4: Implement
Staff are empowered to test out ideas and new ways of working. BLCs ensure a two-way dialogue with senior management and support local tests of change. They can also ensure there is a clear and transparent prioritisation process to articulate what will and will not be actioned to align expectations.
Step 5: Close the loop: confirm it works
One of the most important components of the BLC methodology is ‘closing the loop’ and systematically feeding back to staff and patients changes made because of their engagement. Various mechanisms are used to feedback insights and changes to staff, including biweekly learning forums (to share learning and problem solve together) and visual management tools (to celebrate success and showcase progress).
Who can be a BLC?
BLCs are drawn from a range of diverse professional backgrounds. A clinical background is not a pre-requisite for the role, in recognition that great ideas can come from outside the conventional team. What is more important is observational skill, an interest in processes and systems, and commitment to the learning and improvement ethos.
The BLC role itself is a very flexible model that can be adapted to meet the needs of a department or organisation.
Additional resources:
- BMJ Quality and Safety paper: Description of the BLC role, how it was implemented at the NHS Nightingale Hospital London and practical considerations for introducing the BLC role into an organisation.
- Learning Systems: Managing Uncertainty in the New Normal of Covid-19: A summary of the learning health system approach adopted at the NHS Nightingale Hospital London.
- The five features of a successful Learning Health System: Blog post summarising five core principles that underpin success of LHSs.
Find out more about how we support organisations to implement a learning health system approach to learn and act fast to drive improvement here.