The five features of a successful Learning Health System
Leading global healthcare providers are distinguished by two key characteristics: they learn faster than others, and they implement their learning more reliably and more accurately than others.
The pandemic reinforced how critical it is for NHS providers to have a robust learning process. During the past 18 months, healthcare systems have had to cope with the immense challenges of dealing with the unknowns of a new virus spreading at speed within the population, requiring them to respond and react under intense pressure and uncertainty.
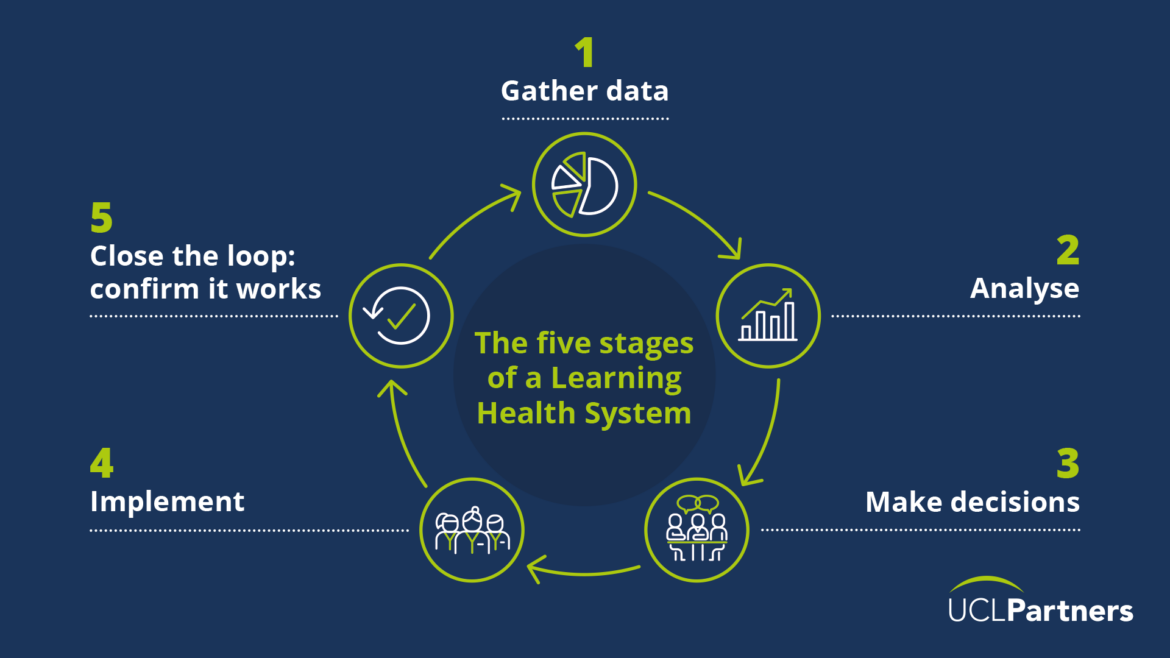
The Learning Health System approach provides a structure for teams, organisations and systems to gather insights and adapt as necessary to deliver the best outcomes for patients, the population and staff. It covers multiple domains, including clinical, operational and staff well-being, and is based on five stages: gather data, analyse, make decisions, implement those decisions, and close the loop by monitoring effectiveness of the changes implemented.
Throughout the pandemic, at UCLPartners we’ve been working with teams to use the Learning Health System approach at all levels within the healthcare system, from hospitals, integrated care systems (ICS) and at regional level. Our work has identified five core principles that underpin a successful learning health system.
1. Identify known areas of uncertainty
Within the pandemic, teams have been able to align quickly on priorities for learning, given the initial unknowns of the virus, how to treat it and the implications for other service changes to mobilise resources to areas of need. Alignment on the unknowns or focus of learning is equally required as the system moves to reset and recovery and as the foundation on which to build a learning system.
2. Focus on helping staff to help the patient and reduce the burden on frontline staff
For example, as part UCLPartners’ work, we visit sites, interview staff and stakeholders and talk to patients, as well as review data to gather perspectives, understand what is working well, what is more challenging and identify new ways of working. By taking the time to listen to those directly delivering or receiving care services, we are better able to understand the impact of decisions in practice and make recommendations for changes where needed.
3. Learn from every single patient or person
Every contact should count, and should be considered a learning opportunity, and acknowledging and facilitating that is part of the wider culture required to make a learning system successful. At NHS Nightingale London Hospital, the Learning Health System approach included the creation of the Bedside Learning Co-ordinator role to help gather insights from the front-line in a systematic way to embed continuous feedback and insight gathering.
4. Associate all practice changes with a rapid feedback loop.
Rapid feedback is required to ensure changes are implemented successfully, acceptable to staff and patients and fundamentally address the route problem they were trying to fix. For example, as part of our Learning Health System for the London Vaccination programme we analysed interventions to increase COVID-19 vaccine uptake in the capital. This involved identifying and exploring reported barriers to vaccination, strategies and interventions to address these barriers, as well as the adjustments to service delivery models to improve access to the vaccine.
5. Concentrate on organisational culture
The five stages of the learning health system – Data, Analysis, Decision, Implementation, Closure – do not work in isolation but need to be underpinned by an organisational culture that is committed to learning fast and acting fast on the agreed areas of uncertainty. The ability to learn should be embedded in the structure and processes at every level and reinforced through the culture and behaviour of staff and leaders. Staff need to be given support and permission to speak up, act and celebrated for their contribution.
Looking ahead
As Integrated Care Systems take on their statutory form, in the midst of what is set to be a difficult winter, there has never been a greater need to embrace better ways to understand evidence and analyse data, to evaluate change and impact, to learn from qualitative insights from staff, patients and the public, and to rapidly share learning in innovative way to deliver improvement. Building on our existing projects, we look forward to applying this approach to the roll-out of Community Diagnostic Centres across London to help improve access to potentially life-saving tests for the population.
The Learning Health System approach provides a framework for teams, organisations and systems to live up to the ‘learn fast, implement learning fast’ ideal to the benefit of patients, staff and the public.
This blog was originally published in the HSJ
Find out more about UCLPartners Learning Health Systems work