Blood monitoring during a time of crisis – from lockdown to go live in a month
At the end of April during Multiple Sclerosis (MS) Awareness week our start-up company NeuroResponse launched a new service to support people living with MS who continue to need their bloods monitored at this time of crisis. The service was created at pace, by a coalition of the willing, fuelled on coffee interspersed with exercise to keep the heart and soul on track. Exactly four weeks from the announcement of lock down we went live.
Impact of COVID 19 on those living with MS
The arrival of COVID-19 changed the world. It makes us all feel vulnerable. For people living with a long-term neurological condition like MS it brings an added layer of anxiety and worry: what it means for their ongoing care, and where and how they will access important services. This includes the blood monitoring required when on a disease-modifying drug.
With the start of the COVID-19 era, the hospital model of care was suddenly stopped as non-urgent NHS services closed and MS specialist staff were deployed to other clinical areas.
Community services have become more important than ever, however after years of underfunding gaps in care for people living with long term conditions such as MS have become more obvious.
The challenge
Recently, the Association of British Neurology advised that blood monitoring for MS patients on disease-modifying drugs could be extended, with a warning that patient themselves must monitor their symptoms closely.
This eminence-based guidance coupled with the absence of support for our already vulnerable patient group posed a challenge to the NHS and people living with MS. Faced with this challenge NeuroResponse explored solutions to maintain an MS blood monitoring service during the pandemic. We began by asking the following questions:
- Do patients want a service that includes home visits?
- Do clinicians want a service?
- Is there anything out there already that we could use?
- Can we offer an @home phlebotomy that complies with Covid-19 isolation guidance?
- Who in our network has the skills and capabilities to help us?
- Can we create a model that does not use scarce NHS resources?
- Can we create a model that enhances NHS resources?
- Could we do any of this in a safe and agile way?
Yes we can!
One of the challenges raised was that whilst people with MS may not meet the criteria for ‘shielding’ as set out by Public Health England, they are at an increased risk of becoming unwell if they develop side effects associated with their drug regimes. Both clinicians and patients thought that it would be useful keep the monitoring programme in place if possible
An @home self-collect blood kit is available from private clinics across the UK. We worked closely and collaboratively with The Doctors Laboratory for a number of years offering timely diagnosis for urinary tract infections . We discussed options with them and identified a kit available locally. The challenge of creating a home phlebotomy service was also discussed with our colleagues in The Doctors Laboratory who helped us identify a highly skilled phlebotomy work force who had capacity. The phlebotomy team, who work with elite Olympic athletes and government industries had capacity to join our service
Creating a team
The next step was to create an infrastructure to support patients as they joined the new digitally enabled service. Our highly valued long-standing partner London Central & West Unscheduled Care Collaborative (LCW) and NHS 111 colleagues helped us to create a new workforce of Patient Engagement Officers (PEOs) from a pool of medical students. The role of the PEOs is to support patients to sign up to the new digital service and triage results to specialist teams as required. We are lucky to have such a talented team meeting the needs of our patients.
We also worked with colleagues in NHSE London and Healthy London Partnership to create clinical and safety governance frameworks and had fantastic support from IT colleagues in The Royal Free London NHS Foundation Trust to create new digital care pathways on our NeuroResponse platform. We linked to networks of Data Protection Officers (DPOs) from across London Trusts to agree information governance frameworks. We reached into our local Integrated Care System leads (ICS) to explore funding opportunities – a work in progress – and asked champions in the NHS system to help us navigate the lakes of bureaucratic treacle: an ongoing journey! We linked to the UCLPartners commercial team and received encouragement and commercial support, including introducing us to a mentor for advice and guidance. The result is that within four weeks of lockdown being announced we were delivering a home phlebotomy service and leading a proof of concept study to test the use of self-test kits @ home.
A professional, kind, friendly service
We created a home phlebotomy service for the COVID-19 era as described in the 3-minute video below.
The @home phlebotomy service is up and running, results are getting back to the specialist teams and they are very pleased with the safety net we offer to them and their patients. Patients love the @home service and have provided positive feedback, including:
- “ L…. was very kind and considerate. She was also professional and explained the procedure to me which I really appreciated. She was wearing full protective (PPE) which made me feel very safe.”
- “Warm professional friendly service.”
- “Excellent service by L…… Set up [and] communication all 1st rate.”
- “Very friendly, professional and reassuring. Thank you!”
- “I [am] happy with the service provided and would like to continue as long as the virus issue exists”
- “Fantastic service – would thoroughly recommend it to anyone. Thank you!”
As mentioned , our new service also includes testing of home self-monitoring kit delivered by post. A proof of concept study to test if a TDL TINY SAMPLE kit could be used by people with MS at home is ongoing. We applied to InnovateUK to test with a wider cohort and will collaborate with colleagues in the Institute of Neurology (IoN) and Professor Steven Hilton at UCL to create bespoke components as required.
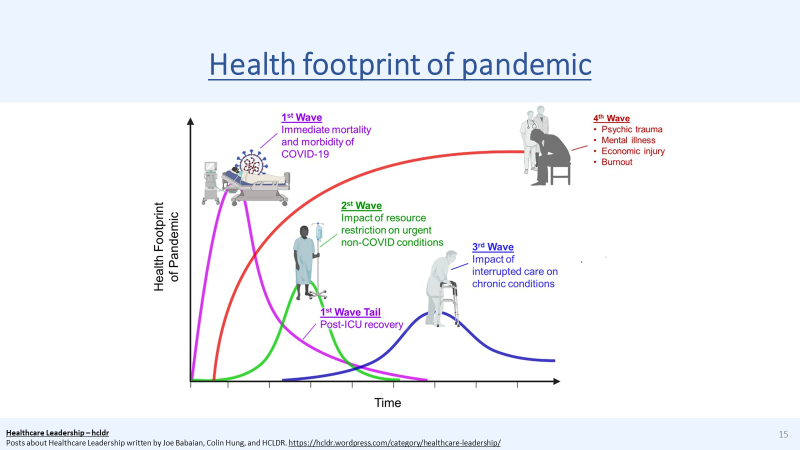
Our values drove us to create a better way to care. We passionately believe that we should try hard to stay close to our patients and do our best to prevent them getting caught up in the predicted tsunami third wave of this terrible pandemic.
We have a long way to go and will not get everything right, but we will keep our nerves of steel to give it our best.