NHS Improvement (NHSI) defines non face-to-face activity as:
Time spent by healthcare providers reviewing and advising a patient on care without that patient being physically present.
Essentially, the face-to-face consultation between a clinician and patient is removed.
You’ll find further definitions on Nf2f activity in the NHSI Approved Costing Guidance.
What are the different types of Nf2f clinics?
Nf2f models can be categorised as either Synchronous or Asynchronous.

Synchronous |

Asynchronous |
| In a synchronous model, the patient and clinician interact in real time. (Royal College of Ophthalmologists, 2016) | In the asynchronous model, the patient and clinician interaction occurs at different times. (Royal College of Ophthalmologists, 2016) |
| For example, via a webcam or phone call. | For example, secondary care specialists make decisions about a patient’s management based on quantifiable data gathered in primary care. Normally, patients are notified of the outcome from this clinic via an agreed communication channel. |
What is a synchronous Nf2f clinic?
Synchronous Nf2f clinics consist of a pre-booked telephone or web-based session – for example, a Skype (video consultation) that replaces a face-to-face attendance. Normally, the clinician contacts the patient, or they will meet at a pre-arranged time on the web-based session.
Examples of synchronous Nf2f clinics include:
Skype consultations
For diabetes care at Barts Health NHS Trust, Skype consultations have replaced f2f consultations between clinicians and patients. Evaluation has demonstrated an improvement in “did not attend” rates, improvement in HBa1c levels – although not statistically significant – increased productivity and patient throughput.
Telemedicine clinics
Telemedicine clinics set up in rural north Wales used both video and telephone consultations to provide frail patients with care closer to home. These clinics reduced the number and duration of consultations, as well as travel time and costs for both patients and consultants. Patient feedback was positive and the concept proved to be a viable option for outpatient consultations in frail, older individuals.
- 20 per cent of outpatient department follow-up consultations (96 in total) were converted to telemedicine.
- There was a 50 per cent reduction in the number of consultations per patient – most were discharged to follow up – and there was less movement of patient notes.
What considerations are there for synchronous Nf2f clinics?
To implement a synchronous model, you may want to consider the following points:
- In most instances, the synchronous model is technology dependent and reliant on an effective network connection.
- Patients have to be digitally literate and able to access the chosen platforms.
- Communication is key – interacting and communicating with patients through synchronous models requires different skills to traditional f2f scenarios.
- How will we consider patient consent, capacity and continuity of care? The GMC and this resource provide some ethical guidance on these issues.
- Safety netting considerations include understanding what systems need to be in place to provide safe monitoring and follow-up despite patients not being seen face-to-face. This ensures that a patient with unresolved or worsening symptoms knows when and how to access further advice.
What is an asynchronous Nf2f clinic?
There are two types of asynchronous Nf2f model. These are defined below:
Clinical review or a multidisciplinary clinic review
This model is usually initiated following a referral from primary to secondary care. However, this referral might sometimes start in secondary care – for example, at a virtual fracture clinic. A clinician or a multidisciplinary team of clinicians will review notes, investigations and quantifiable data – without the patient being present. Following review by care specialists, there may be three possible patient outcomes:
- Discharge back to primary care and management by their GP.
- Collaborative management via this virtual model, where secondary care specialists and the GP work together to manage patients collaboratively.
- Referral to the face-to-face clinic.
Normally, the patient is contacted by primary or secondary care to be advised of the outcome and the proposed management plan.
Online portals and apps
These systems enable patients with long-term conditions to record their symptoms into an online portal. Secondary care specialists use this patient-generated data – and possible investigations undertaken in primary care – to consider their condition.
If the patient is managing their condition well and they are clinically stable, no further review is required. Additionally, if escalation is needed, standard operating procedures should enable this.
Examples of asynchronous Nf2f clinics include:
Virtual e-clinics for chronic kidney disease at the Royal London
GP refers patients to a Royal London “CKD virtual clinic” where a secondary care specialist reviews the patient record, which includes data generated in primary care. This clinical review enables the specialist to advise on the management of CKD patients who are referred to the service. Management may be provided in one of the following ways:
- Through this virtual model.
- Discharge back to the GP with advice.
- Referral for face-to-face review.
This model has seen a reduction in waiting times for an outpatient appointment fall from between 55 to 84 days, to five days. It has also led to a 20 per cent reduction in f2f outpatient appointments. (Royal London)
Web-based patient management portal at East Surrey Hospital
The Patients Know Best (PKB) portal enables an Nf2f delivery model that allows patients to record symptoms within the system and communicate remotely with the IBD team. The portal provides timely access to teams and prompts escalation where necessary. Patient access to specialist care at the time of a flare-up has reduced from six weeks to one week. There’s also been a reduction in the number of hospital admissions and outpatient appointments. (RCP, 2018)

What are the considerations for asynchronous Nf2f clinics?
To implement an asynchronous model, you need to consider the following points:
- The asynchronous nature of this model means that clinician and patient interaction occurs at different times. Communication with the patient about their management is vital to ensure that they’re well informed.
- Asynchronous models may need interoperable systems that, in turn, require the planning of integrated IT.
- They rely on the availability of appropriate information when the clinician reviews patient data.
- How do we consider patient consent, capacity and continuity? The GMC and this resource provide some ethical guidance on these issues.
- Safety netting considerations: what systems are in place to provide safe monitoring and follow-up despite patients not being seen face-to-face? This ensures that a patient with unresolved or worsening symptoms knows when and how to access further advice.
How do Nf2f differ from advice and guidance?
Advice and guidance is a basic form of an Nf2f model. It enables clinicians to seek advice from one another. A national Commissioning for Quality and Innovation (CQUIN) indicator has been established to incentivise providers to set up and deliver these services. Consequently, it has its own nationally agreed funding arrangements, whereas NHSI have published non-mandatory tariffs for Nf2f activity.
We are not aware of any work to understand how the models differ, and how they are complementary in today’s health system. However, we believe there are a few key differences between the models:
- Usually, advice and guidance will not have access to integrated health records – for example, the ability to view primary care data in secondary care. Therefore, this means that advice and guidance is given, based on the information provided by the requester.
- Responsibility for the patient clearly remains with the clinicians making the advice and guidance request.
- In most cases, the referral guidelines or criteria set for advice and guidance are less strict than those for Nf2f clinics.
- Consequently, Nf2f clinics are usually set up around a formal diagnosis or symptom group. Advice and guidance may be much broader.
We recommend engaging with your commissioners to ensure that proposed Nf2f models complement any pre-existing or planned advice and guidance services.
Is there any guidance on whether Nf2f clinics are appropriate for us?
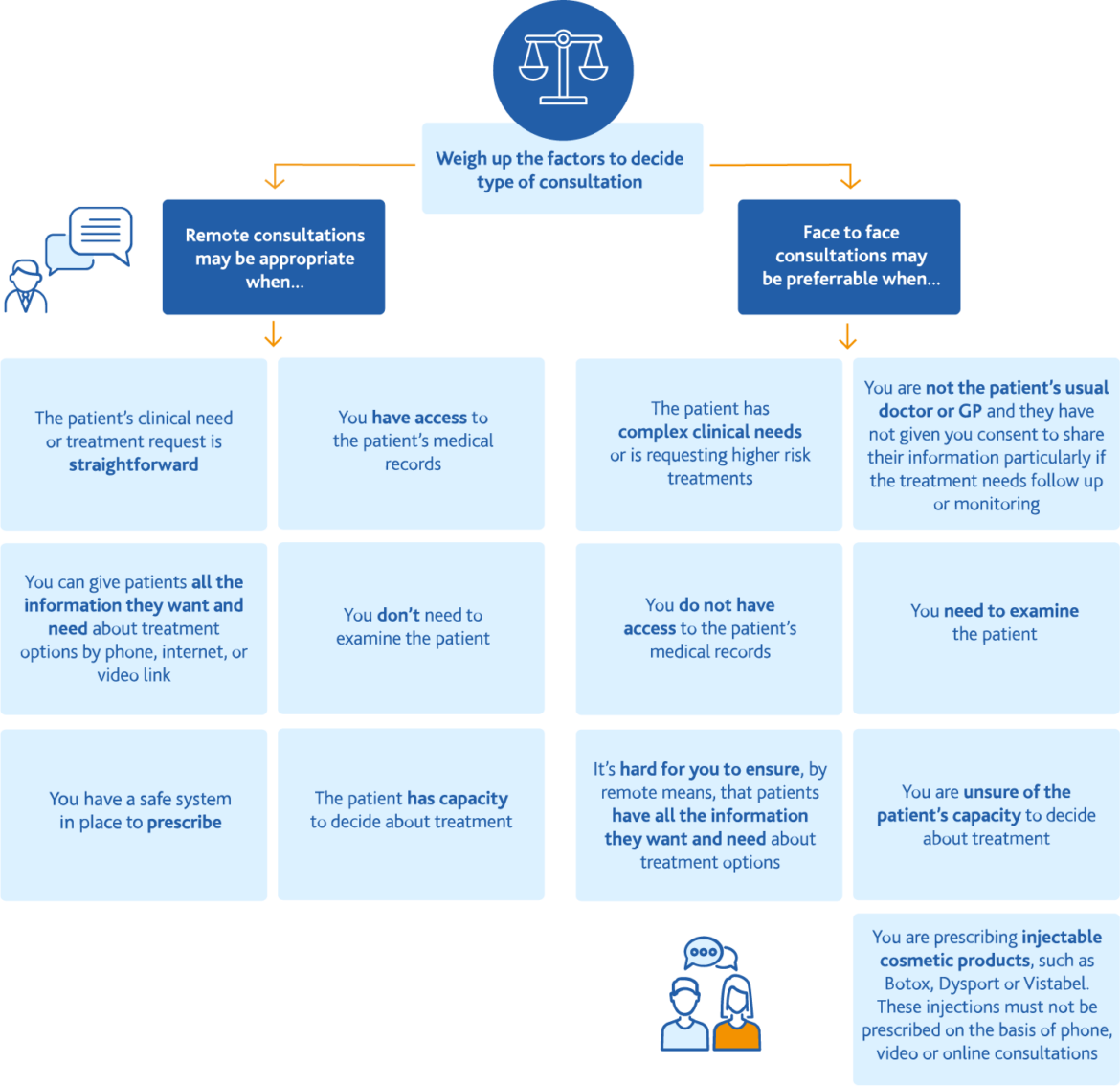
The GMC have produced an infographic to help determine whether a remote consultation is appropriate: