Whether the idea for an Nf2f clinic has come from clinicians, service managers, or senior management, planning and justifying your proposed new model of care is an essential first step towards setting it up.
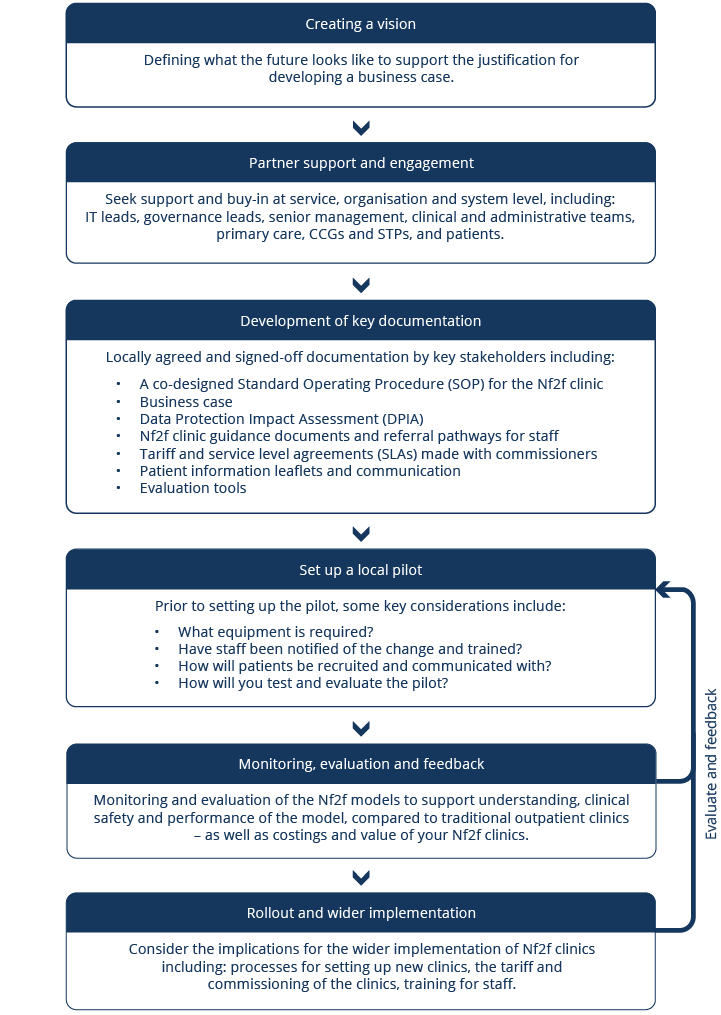
This section encourages you to consider the steps required throughout the process – from developing a vision and achieving stakeholder buy-in and piloting the clinic, to rolling out your Nf2f model more widely and evaluating its impact.
This process map has been adapted from Barts Health who developed it for virtual video-based consultations.
Process map for setting up non-face-to-face clinics

What is meant by defining a vision – and how do we create one?
A vision sets out what the future might look like. It also defines the endpoint of a change process, without specifying the actions required to reach that endpoint. Creating a vision provides the building blocks to help plan the desired change. It enables you to communicate, at a high level, why and how you should deliver Nf2f clinics. A vision also supports conversations with key partners to help buy-in for a collaborative approach.
NHS Improvement (NHSI) guidance around creating a vision for change includes setting out three key stages:

Set parameters and boundaries for the vision

Support a group to create the vision

Share the vision with others
With your colleagues, consider the guidance and think about how you create your vision for Nf2f clinics. In collaboration with colleagues, you’ll also need to consider the justification for developing a business case. Together with the vision, the business case gives stakeholders evidence that supports your reason for change, and the expected benefits. These benefits can include improvements to quality of care, patient experience and any financial implications.

Which stakeholders do we need to engage and seek support from?
Buy-in is essential at a service level, across your organisation and the wider health system. This means that you must engage with colleagues who have a vested interested in the project. For example, you may wish to engage with:
- Wider clinical and administrative teams
- Primary care
- IT department and information governance leads
- Finance
- Governance leads
- Estates leads
- Service managers
- Commissioners and the STP
- Patients
You’re seeking support from these stakeholders for the implementation of an Nf2f clinic. When you plan to engage, it’s important that you allow plenty of time for discussions about how Nf2f clinics will affect the service and patient care.
It’s also important to consider that NHS Trusts and Clinical Commissioning Groups have a legal duty to engage and involve the public and service users in certain decisions that affect the planning and delivery of NHS services. This would include the delivery and implementation of Nf2f clinics as this is likely to involve changes to pre-existing services.
How do we monitor stakeholders and keep them informed?
Nf2f clinics have the potential to impact a range of stakeholders across the system. You may wish to undertake a stakeholder mapping exercise to identify the key figures. You should determine their influence and interest to think through how to keep them informed and support the development of a communications plan. This can be done using a stakeholder analysis and communications plan template. You may also wish to consider their roles and responsibilities when supporting your project – and any leverage you may have when working in collaboration with them.
What about project management?
To support and drive the development of your Nf2f clinic, in partnership with clinical colleagues and the wider system, you must also achieve buy-in for project management support. This should include allocation of dedicated project management resources to support the development and launch of your project. They will also be able to support the effective operation of the Nf2f clinics.

What documents do we need in place and signed off?
In this step, you need to bring together a range of documents to support the planning process and ensure that there’s an appropriate audit trail for governance. These documents include:
Co-designed Standard Operating Procedures (SOPs) for the Nf2f clinic
Locally agreed and signed-off business case
- Written to support potential changes to your services from a business perspective and the implications on the trust.
- This should include estate considerations to ensure that sustainable solutions are planned collaboratively and agreed.
Data Protection Impact Assessment (DPIA)
Nf2f clinic guidance documents and referral pathways for staff
Tariff and service level agreements (SLAs) made with commissioners
Patient information leaflets and communication
Evaluation tools
Within the business case, if relevant to your model, you may also wish to consider other aspects of the integrated pathway. For example, planning for the funding to contain administrative resources (including project management) and other health professional resources such as nursing or phlebotomy.
When you build a business case, consider each key area found within the following example structure.
The subsequent sections will support you in considering the local implications for the above documents and resources.

When should we run a local pilot for a new Nf2f clinic?
When your documents are in place, and all governance is taken into consideration, you can plan a local pilot of your clinic.
By testing on a small scale, you ensure the change is safer and less disruptive for patients and staff. Using the Plan, Do, Study, Act (PDSA) cycle and model for improvement provides a framework for developing, testing and implementing changes from the Nf2f pilot. Furthermore, it facilitates building on the learning from PDSA cycles in a systematic way before wider rollout and implementation. This cycle is recommended by NHSI when planning any improvement or change to work processes. This process should include the team to ensure that all relevant information is shared.
Some key considerations before the pilot starts are:
- Do you have the correct equipment in place (for example, IT systems)?
- Have staff been trained and notified of the change?
- How will patients be recruited into the pilot and communicated with?
- How will you test and evaluate the pilot?

Why do we need to consider monitoring, evaluation and feedback?
Monitoring, evaluation and feedback is a continuous process that starts as soon as the pilot is up and running, through to the wider implementation and rollout of the clinic.
It’s important to plan for evaluation at the start, as there’s often a resource implication associated with it. This ensures that appropriate project costs are allocated to measure the impact of the Nf2f clinic.
Monitoring and evaluation supports understanding:
 Clinical safety of the Nf2f model |  Performance compared to traditional models and evidence |  Costings and value |  Ongoing learning and implementation |
| By monitoring whether the Nf2f model is clinically safe. | By measuring the performance data for your Nf2f clinic compared to traditional models of care, you can also contribute to the growing Nf2f evidence base. | By understanding the cost of this new model versus the traditional model of outpatient care, does this represent good value for money? | Studying and developing the model, during implementation, helps us learn about and refine the service to meet local needs, as well as determine whether we should introduce this model more widely. |

At this stage, you will have run a local pilot, evaluated it and potentially decided to implement more widely across your service, other specialities, your trust, or region.
This will require more teamwork to determine the process of rolling this out and wider implementation. You may wish to consider and agree:
- Tariffs for each of the models.
- Processes for setting up new clinics.
- IT and integrated system solutions.
- How local services will co-design and adapt Nf2f approaches for their service.
- Re-evaluation after wider implementation to ensure outcomes are comparable (include qualitative data such as clinician and patient feedback).
- Continuous staff training on how the new clinic is run.
Remember, testing and adapting the Nf2f model across the range of settings is important to allow for continuous improvement.