What are the drivers behind the move to Nf2f clinics?
A report by The Royal College of Physicians has identified that, on a national level, NHS outpatient hospital visits have nearly doubled in the last decade.
These visits account for 118 million consultations a year in England alone.
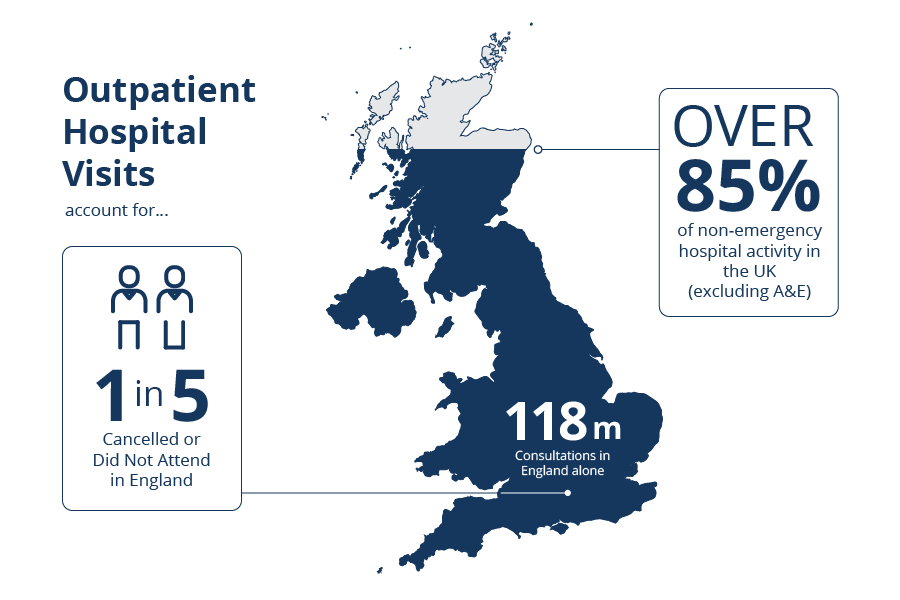
These appointments account for a large percentage of non-emergency hospital activity, excluding A&E. Despite a range of initiatives to improve efficiency at both national and local levels, one in five outpatient appointments in England is cancelled or reported as “did not attend”.
The report also highlights that 5% of all road traffic – 1 in 20 journeys – in England is NHS related travel. This contributes to reducing air quality, which has a direct impact on people’s health. It has been estimated that NHS related traffic is associated with:
- 753 deaths from air pollution.
- 8,844 life years lost from air pollution.
- 85 deaths and 722 major injuries from accidents.
- £650 million in NHS expenditure.
This all results in a huge cost and burden not only to the NHS, but also to the environment, making the traditional outpatient model outdated and unsustainable.
How do the NHS plan to tackle this?
Data suggests that many traditional outpatient appointments are not required. As a result, the NHS Long Term Plan promotes:
…the adoption of new, digitally enabled, models in primary and outpatient care.
Through outpatient transformation, the NHS has set a target of avoiding up to a third of face-to-face outpatient visits during the next five years. This will remove the need for up to 30 million outpatient appointments each year.
Additionally, the Topol review was commissioned by the Secretary of State for Health and Social Care to explore how to prepare the healthcare workforce, through education and training, to deliver a digital future. The review highlights how technological developments are likely to change the roles and functions of clinical staff during the next two decades. It also recognises the need to:
…prepare the workforce for embracing new ways of working with technology to address the increasing demand on health and care service.
The NHS Long Term Plan, RCP report and the Topol review, all acknowledge that Nf2f approaches are a potential solution to addressing the system-wide issues facing the NHS.
Watch the animation below to see how Nf2f models are expected to help achieve the aims laid out in the NHS Long Term Plan.
Now that we understand the national drivers, how do we identify local drivers?
Start by considering local issues within our health and care system. Look for issues that illustrate and emphasise a need for outpatient transformation and the implementation of Nf2f solutions.
Although local drivers for outpatient transformation will be specific to each area, they may include some of the following issues. Consider each of the areas below then click to reveal why it might represent a local driver.
Outpatient demand and capacity
Increasing demand and reducing capacity on particular outpatient services in your area mean that alternative models to face-to-face appointments can offer a solution.
Demographics of your populations
An ageing population, or an increase in prevalence of particular long-term conditions in your area, can drive a need for outpatient transformation.
Patient experience
Improving patient experience by reducing the requirement for them to travel to hospital, paying associated costs, taking time off work and arranging cover for care commitments.
Managing patients with co-morbidities
Developing more effective ways of managing patients with co-morbidities.
Collaboratiative and integrated approaches
A need to work towards a more integrated approach between primary and secondary care, to improve patient care through more effective and efficient ways of working.
Reducing your carbon footprint
Local environmental factors and a need for more sustainable models of healthcare might lead to a reduction in carbon emissions.