UCLPartners search tools could help primary care save lives through improved cholesterol management, new data suggests
Our local insights have been echoed in the newly published national audit data for cardiovascular disease (CVD) prevention, which shows around one in five people living in England, who have had a previous heart attack or stroke, are not on the NICE recommended statin treatment to their lower cholesterol. The UCLPartners’ data also shows that 60% of people with CVD are on statins, but not at the recommended dose.
Raised cholesterol is one of the leading causes of heart attack and stroke, common conditions that account for a quarter of premature deaths and 25% of the life expectancy gap between most affluent and most deprived communities. National modelling for the NHS Long-Term Plan in 2019 showed that systematically tacking the under treatment of cholesterol along with blood pressure and atrial fibrillation would prevent 150,000 cardiovascular events in ten years.
In practice it has been difficult to get an in-depth picture of gaps and opportunities in cholesterol treatment to prevent CVD because there is very little information about cholesterol collected in established data sources, such as the QOF.
Our Proactive Care Frameworks (PCFs) provide an opportunity to overcome this and generate some real time insights into how improvement in cholesterol-lowering treatment could prevent heart attacks and strokes at scale. For individual practices, the PCFs stratify patients with CVD so that clinicians can easily identify and prioritise people whose treatment needs to be optimised. This may include initiating statins, increasing dose or intensity of statin, or for those people on maximal statin regimens it could be initiating newer therapies such as Inclisiran, Bempedoic Acid or PCSK9 (mab) inhibitors.
We worked with one ICS in London and one in the east of England to apply our PCF tools across the healthcare records of 2.8 million people. We found that most people living with CVD are not on the recommended treatment. Detailed analysis of 100,000 people who have had a previous heart attack or stroke showed one in five are not on a statin, three in five are on a statin, but their dose is not optimal, and significant numbers of people are on maximal statin therapy, but their cholesterol levels remain above target.
To delve further into this finding, we used the data to extrapolate what the local Size of the Prize would be were ICSs able to optimise treatment of high cholesterol. The numbers are huge.
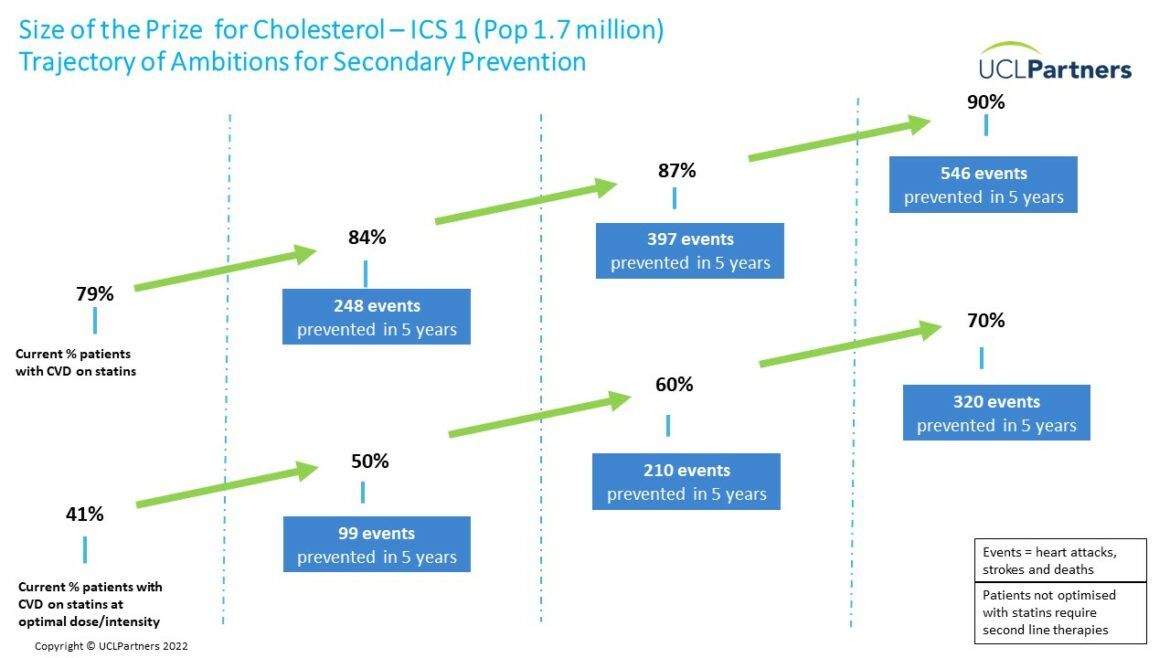
In the example above, which is focused on only one ICS area in London, if improvement led to 90% of people with CVD being prescribed a statin and 70% taking optimal doses, we could prevent over 800 strokes and heart attacks in five years. This would save many lives, reduce admissions to hospital, and cut costs to the health and social care system.
Dr Matt Kearney, Executive Clinical Director for Cardiovascular Health at UCLPartners and general practitioner said: “High cholesterol is widely recognised as a major risk factor for life threatening cardiovascular events such as heart attack and stroke. Yet our management of the condition could be a lot better. This is partly down to historical statin hesitancy, but it is also because we have lacked the data to help us see the scale of the problem and the scale of the opportunity in tackling high cholesterol.
“The UCLPartners Proactive Care search tools, available free for every practice, primary care network and ICS, can provide this data, identifying patients who are on no treatment or suboptimal treatment, and risk stratifying them so that those with greatest need can be prioritised. We have used the data generated in 2 ICSs to model a Size of the Prize for cholesterol to understand just many strokes and heart attacks can be prevented at different levels of ambition.”
Access the UCLPartners Size of the Prize for Cholesterol slide set.