Simulating EPR in Healthcare – part 1
Paul Wilder (Interim lead for Technology Enhanced Learning at Frimley Health NHS Foundation Trust)
The Electronic Patient Record has changed dramatically over the last 20 years as NHS Trusts start embracing computer systems to record details about the patient’s medical journey (nursing/medical notes, radiology, clinical observations on NEWS 2, prescribing, etc). As simulation technologists and educators our challenge is to incorporate a representation of these systems effectively and smoothly into our scenarios.
For many years every simulation I supported had a whole set of paperwork, that we either laid out in the scenario room in the patient folder at the end of the bed for the candidates to look through to see the patient history, or was hidden in various locations that we would inform the candidates about once they had completed the appropriate clinical task e.g. the doctor would consent the patient manikin and role-play taking an ABG with a prop; when the facilitator decided it was appropriate, we would use our microphone to inform the candidate over the room speaker that their ABG results were back and could be found under the blue tray by the mirror.
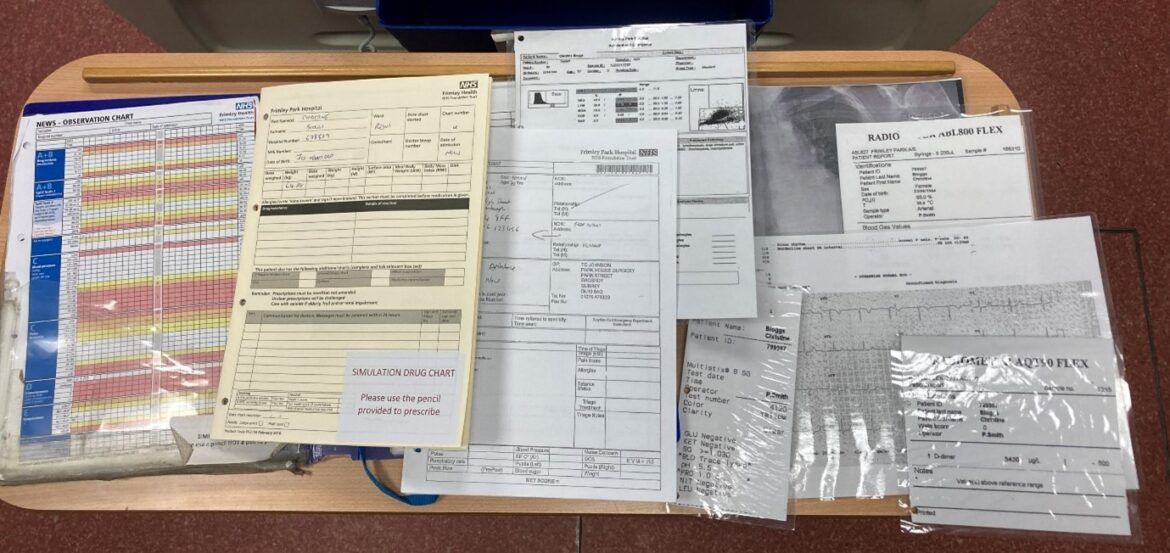
Below is the paperwork from one of our scenarios – a NEWS sheet, Drug chart, CAS card, PoC bloods, VBG results, X-ray, ECG and so on. This used to roughly approximate how our trust dealt with real patients until we got an EPR several years ago, but I knew the fidelity of our simulations was really in trouble when a medical student during a scenario looked at our paper Drug chart and said they had never seen one before and didn’t know how to use it..!
So the main options a simulation service has in this regard is, I believe:
• Carry on using paperwork
• Real EPR training solutions
• In-house solutions
• Commercial solutions
Hopefully you will quickly rule out the first option of just ignoring the problem, because it’s not going away and as simulation technologists we should always be striving to mirror reality as much as possible in our scenarios, bearing in mind our educational objectives, costs etc, of course.
The second option involves the use of the training systems that many of the modern EPR systems provide, including Cerner, Epic and Rio.
Although this might be the real system in use in your trust and thus free, there are a number of disadvantages of this approach, the most obvious of which being that in the majority of our simulations the educational objective does not include teaching candidates how to use what is a complicated EPR system – indeed it could well prove to be a complicated distraction and provide ‘cognitive overload’ to the candidates in what was meant to be a simple scenario. In addition, these systems are often not controlled by the simulation service and thus likely to prove inflexible for our scenario needs e.g. you might only be able to use the patients provided and not create your own or even be unable to alter anything on the ones that are provided.
The third option of creating your own in-house solution is one some have gone down and in theory is a cost-free option, but in reality involves skilled staff members programming, and the results are dependent on the amount of time spent creating them, which can be considerable. Establishments that have gone down this route that I talked with were Purdue School of Nursing, RSCH, ASPH, UCLH and Bishop Auckland Hospital.
In the second part of this article I will briefly discuss their different approaches to creating an in-house simulated EPR system, and then go on to examine a commercial system specifically created to replicate an EPR system for Healthcare simulation, and how it deals with the various challenges raised by running in an educational setting.