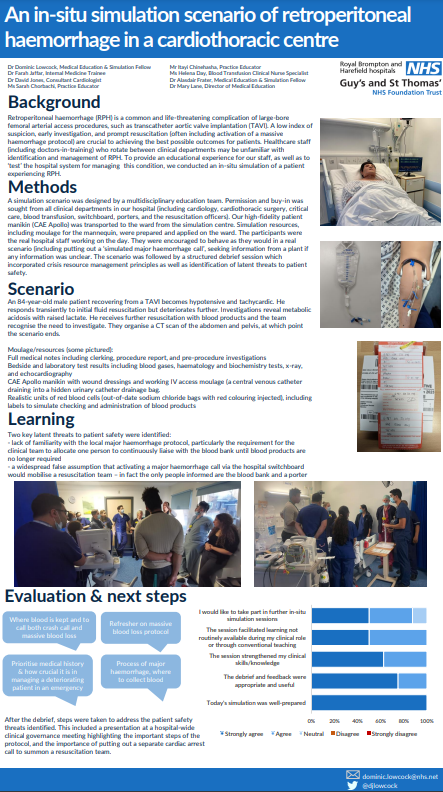
Retroperitoneal haemorrhage is a common clinical problem encountered in our cardiology service as a complication of large bore vascular access in the Heart Lung & Critical Care Clinical Group as part of Guy’s & St Thomas’ NHS Foundation Trust. It is not only difficult to recognise due to non-specific presentation, but it can also carry high morbidity and mortality if treatment is delayed. Furthermore, it requires a complex multisystem and multidisciplinary hospital response to achieve good outcomes for patients, which increases the likelihood of communication and logistical errors. We saw an opportunity to design a simulation scenario to identify latent threats to patient safety in the system response to this condition, as well as to provide an educational experience to staff involved.
An in-situ simulation scenario was designed with our multidisciplinary education team utilising our high-fidelity patient manikin (CAE Apollo), which was transferred from our simulation centre to a bed space on a cardiology ward on the day of the simulation. Simulation resources and moulage were prepared to improve the realism of the scenario, including working vascular access in the manikin and realistic-looking bags of packed red blood cells in the blood bank and theatre emergency blood fridge so that the whole process of transfusion could be replicated accurately.
The scenario was followed by a structured debrief for the staff taking part, and a subsequent analysis by the simulation team of the latent threats identified. These included lack of knowledge of the major haemorrhage protocol, including the staff summoned by putting out a major haemorrhage call and where emergency blood can be found. These learning points were shared with the whole organisation at a clinical governance meeting.
The project was ambitious but rewarding, and we are hugely grateful for the support of all who contributed including: the Harefield acute cardiac care unit management team and practice educators, the transfusion service, resuscitation officers, switchboard, porters, and staff from all departments who attended (cardiology, cardiothoracic surgery, anaesthetics, and critical care). We received overwhelmingly positive feedback from those who took part and would be very happy to share our experiences further with anybody who is interested.