From Bedside to Courtroom: Transforming Nursing Documentation through Simulation Learning.
Maria Casado, Chief Nurse Improvement Fellow
Oh Manguilimotan, Clinical Practice Facilitator
Beth Tennant, Simulation Manager, Clinical Education
Matthew Judd, Simulation Education Fellow
Paula Anderson, Chief Nurse Information Officer
It is estimated that nurses spend around 25% of their working day documenting care and looking for information (NHSE, 2021); precious time that could be utilised in patient care. Audits of health records and conversations from different nursing team across University College London Hospitals (UCLH) revealed that nursing documentation often contains discrepancies and inaccuracies due to duplication, unnecessary and incomplete information, misalignment with the nursing process (assessment, planning, implementation and evaluation), and lacking rationale behind nurses’ decision-making to patient care.
As part of an improvement project, we developed and piloted a one-day simulation-based workshop that aimed to facilitate reflection and discussion on the importance of effective documentation. The workshop took the nursing workforce through a case study that resulted in a coroner’s court and was inspired by one of the cases we encountered from the future death case reports.
Recognising the apprehensions, negative implications, and risks of simulating a coroner’s court for staff, we ensured psychological safety was attended to throughout the sessions. This enabled facilitation of a learning experience and journey, while also emphasising the role of documentation within healthcare and its importance through the moot coroner’s court. Each activity was followed by a sensitive and reflective debrief to support this process.
The workshop was designed to enable nurses, nurse associates and healthcare assistants to explore and enact real-life practice without compromising patient safety. This was built on their initial perspectives towards effective documentation – which enumerated examples of translation to the clinical setting. The first activity encouraged participants to examine and discuss their own practice. They were divided into two groups to create a collaboration board and explore examples of effective and ineffective documentation, its impact on safety, multi-disciplinary communication, and legal proceedings. The boards were then presented and discussed back in the group.
The case study was then presented through a pre-recorded simulation video portraying the care a clinical team comprising a Healthcare Assistant, a Nurse and a Doctor provided for a patient suffering a fall during a night shift. Participants were encouraged to take notes of any information they considered relevant for documentation.

The group was then divided into groups according to their professional roles and were tasked with documenting all relevant information, or critical moments of patient care, in the training environment of the electronic health record system, using the workflow they usually follow in their clinical areas. This was followed by a debrief which explored barriers and enablers the teams experienced when completing this task.

For the second simulation exercise, the same teams were then supported through the process of writing a legal statement to present in the moot coroner’s court, based on their clinical documentation, featuring professional actors. To preserve psychological safety, the teams were encouraged read the statements and answer questions together, making use of “time outs” for an opportunity to cross-check with their documentation in the system and with each other. A post-simulation debrief facilitated exploration of how the experience was changing participant’s perceptions of the impact of documentation and their ideas to improve practice.
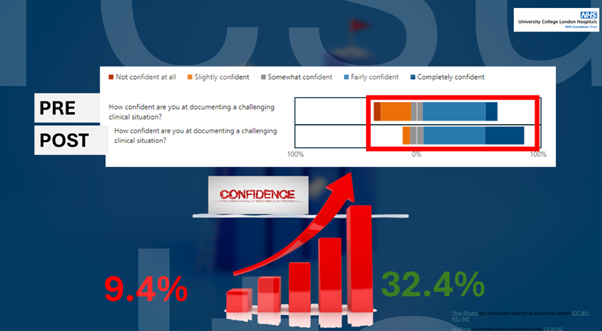
An initial pre– and post-course survey was used for evaluation and measurement of participant confidence in their current documentation practices. It was evident how their confidence had shifted after the workshop, with those self-describing as “completely confident” increasing from 9.4% to 32.4%, alongside emergent themes from qualitative responses outlining intentions to change quality and efficiency of documentation practices.
The workshop also provided greater insight into the systemic and cultural barriers to documentation to support wider improvement efforts and longer-term outcomes, which include roll-out of the workshop trust-wide and making it multi-disciplinary.
We were very proud and fortunate to have presented this project during the UCLH Festival of Excellence 2024 in June, and we, the authors, are hoping to further the discourse on this topic and look into future innovations to enhance the pilot workshop.

If you would like to know more about this learning and improvement project, please contact us in our email addresses below:.
References:
- Bunting J, de Klerk M. Strategies to Improve Compliance with Clinical Nursing Documentation Guidelines in the Acute Hospital Setting: A Systematic Review and Analysis. SAGE Open Nursing. 2022;8. doi:10.1177/23779608221075165
- NHS England. Towards a unified vision of nursing and midwifery documentation . 2023 Available from https://www.england.nhs.uk/long-read/towards-a-unified-vision-of-nursing-and-midwifery-documentation/#references
- NHS England. Why we’re developing standards for nursing documentation. 2021 Available from https://transform.england.nhs.uk/blogs/why-were-developing-standards-for-nursing-documentation/
Acknowledgments:
This workshop would have not been possible without support, guidance and contributions from:
Claire Humphreys – Matron Westmoreland Street Hospital UCLH
Faye Hickey – Ward Sister Urology Westmoreland Street Hospital UCLH
Natalie Dean – Ward Sister Thoracic Westmoreland Street Hospital UCLH
Ferdilyne Bacani – Ward Sister Short Stay/ SAU Urology Westmoreland Street Hospital UCLH
Pamela Stephenson – former Nursing Information Officer UCLH
Katharine Kandelaki – Claims and inquests manager. UCLH
David Hendy – former Deteriorating Patient Lead UCLH
Hannah Perks – Clinical Practice Facilitator. UCLH
Iona Fernandez – Urology SHO, UCLH
Kim Oliver – Thoracic Ward Administrator, UCLH
Grzegorz Drozdz- Trust Falls Lead UCLH
All WMS Nurses, Nurse Associate and Healthcare assistants who participated in the workshop.