Improving care for asthma patients in north west England
Search, stratification and using the wider workforce during the pandemic
The Innovation Agency – the Academic Health Science Network (AHSN) covering the North West Coast of England, is working with GP practices in Knowsley to help improve care of patients with asthma. The team are using the Proactive Care asthma framework developed by UCLPartners. This framework and the principles of the programme have enabled Knowsley Community Respiratory Team to identify, stratify and optimally manage patients in the community.
The Innovation Agency originally presented UCLPartners’ Proactive Care frameworks to local primary care systems in summer 2020. In Knowsley, work had already begun to develop a Knowsley high-risk Asthma Clinic (K-HAC), via the Knowsley Integrated Asthma Service (KIAS). However, The K-HAC model was untenable due to COVID-19 restrictions on spirometry and other aerosol generating procedures. The Innovation Agency worked with the Asthma Lead for Liverpool University Hospitals Foundation Trust and the KIAS team, who modified the UCLPartners searches to make them more relevant to the local population in Knowsley.
This approach, which stratified patients according to need and encouraged digital first approaches, also fitted well with the increase in virtual consultations required in the pandemic to protect patients and staff. The Knowsley team were keen to ensure that the highest-risk patients in Knowsley, living with a respiratory condition, had a review with an appropriate member of the healthcare team and had their treatment plan optimised.
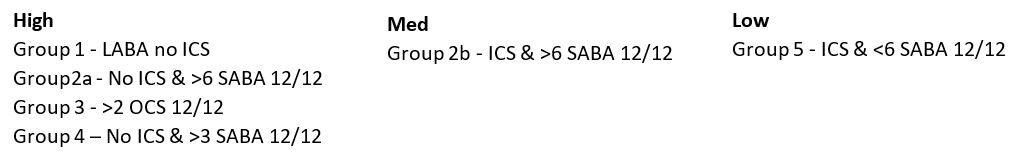
Implementing the framework also provided an opportunity to address the issue of Short-Acting Beta Agonists (SABA) over-prescribing in Knowsley and the team decided to adapt the risk groupings presented in the UCLPartners frameworks in response to the local context.
Implementation
The UCLPartners searches were first run in October 2020 across a GP Federation, Primary Care Knowsley, which comprises 11 practices across three Primary Care Networks, together covering 52,000 patients – a third of the population of Knowsley. Working across one Federation with its shared systems was an important enabler. This meant the Innovation Agency could focus on driving forward the work rather than needing to coordinate stakeholders from several organisations.
Patients were stratified in accordance with severity of their condition and clinics were set up and led initially by the asthma specialist nurses. The nurses then trained other members of staff in the practices.
Clinics were a mixture of virtual and face to face. Face to face appointments were necessary if the nurse was conducting FeNO testing as a measure of how well controlled the patient’s asthma is. The patients in the lowest risk group were sent text messages to remind them of the importance of using preventative inhalers. They were also asked to complete an Asthma Control test to assess their current control.
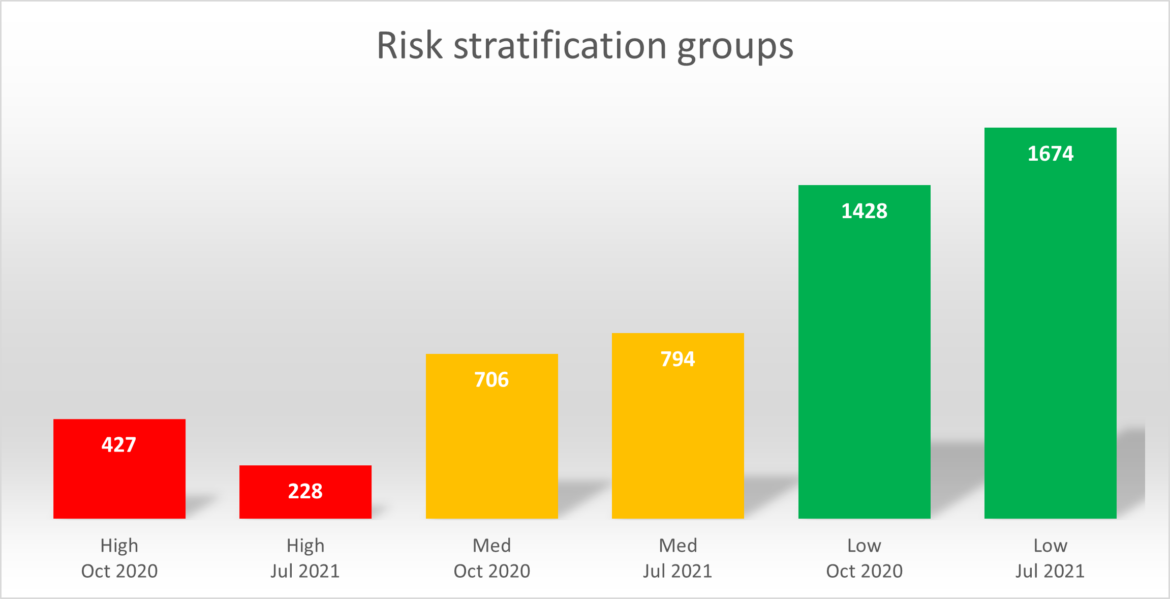
Our goal was to move high risk patients to lower groups to ensure they were stable and optimally managed.
Results
Since the clinics began in October, the following results have been observed:
• 747 patients seen
• 565 face to face consultations
• 71 telephone consultations
• 42 referred for diagnostics
• 221 step-up changes to treatment
• 7 step-down changes to treatment
• 45 device changes
Improvements
Data show that there has been a reduction of nearly 50% in high risk groups. Medium risk has increased by just over 10% and lower risk groups have increased by approximately 15%. There was some patient movement in this period in joining or leaving the practice.
Working with the wider practice teams – the Physician Associate
This model of stratifying patients and optimising digital tools in the management of these patients has enabled teams to work safely with patients in the most need of support. The stratification process also considered which staff were the most appropriate to support the patients, and training for other practice staff was delivered. Due to the encouraging results to date, GP surgeries have agreed to support a Physician Associate programme (in partnership with Liverpool Heart and Chest Hospital NHS Foundation Trust) and have identified and trained Physician Associates to lead the stratification process and run the clinics, whilst being supported by admin teams, health care assistants, nurses and clinical pharmacists.
Training and roll out of the new clinics started in August 2021, overseen by the Asthma Specialist nurse. The Innovation Agency have committed to support the secondment of the specialist for an additional four-month period, enabling the initial cohort of patients to be followed up and making sure that all of the Physician Associates are fully trained, their clinics are up and running, and that the staff in the practices are also supporting the work.
Utilising an integrated team means that the patients are benefitting from a multidisciplinary approach to their care. One of the legacy pieces from this work will be multi-disciplinary team meetings for the Physician Associates to feed back into. Ensuring the continuing best quality care for the patients.
The partnership between Liverpool Health and Chest Respiratory team, the CCG in Knowsley and the five early adopting practices have demonstrated that a partnership approach can help with the reset and recovery work in primary care. The framework is adaptable but upholds principles of: identifying patients in the most need, virtual first approaches, encouraging patient self-management and involving the wider practice teams to support the work.
For further information and the work of the Innovation Agency North West please visit: https://www.innovationagencynwc.nhs.uk/