Detecting heart arrhythmias with FibriCheck app during the pandemic
During the COVID-19 pandemic, Wanstead and Woodford primary care network (PCN) partnered with FibriCheck to co-create a virtual screening approach for at-risk cardiovascular disease (CVD) patients in their population. From October 2020 to March 2021, FibriCheck collaborated with the PCN to couple their flu clinic outreach with remote cardiac monitoring.
While this approach started as part of a harmonised approach to detecting Atrial Fibrillation (AF) – a common type of irregular health rhythm that can increase the risk of stroke – in flu clinics, the pathway was quickly applied to COVID vaccine clinics.
FibriCheck is a smartphone application that allows patients to check their heart rhythm at home without needing any additional equipment. UCLPartners have supported FibriCheck through both the NHS Innovation Accelerator and the DigitalHealth.London Accelerator, to develop their business case and market-readiness.
Challenge
One in four adults develop arrhythmias in their lifetime. This can often lead to stroke, with 4.25 million strokes each year in the UK caused by cardiac arrhythmias. Up to 75% of these strokes could be prevented with timely detection and intervention.
To diagnose AF, a GP often reviews the patient’s signs, symptoms and medical history, and conducts a physical examination, including a pulse check. If there are concerns, the patient will often be offered a 12-lead electrocardiogram (ECG) followed by a holter monitor (a portable ECG device to record their heart’s activity for 24 hours or longer). Other diagnostics include blood tests, echocardiograms and chest x-rays, with referrals to haematologists to prescribe anticoagulation therapy and a cardiologist if they have any co-existing cardiac conditions. Together this amounts to a lengthy and time-consuming process. Added to this, during the pandemic, physical examinations such as pulse checks were challenging to deliver owing to care restrictions and staff redeployment.
In anticipation of the winter flu season and the second wave of COVID-19 looming, the PCN explored digital solutions to relieve the burden and considered including with their annual flu clinics around the East London patch.
Solution
The team at FibriCheck have developed a regulatory-approved and clinically-validated cardiac monitoring solution, as referenced in UCLPartners’ Proactive Care Frameworks for Hypertension and Atrial Fibrillation .
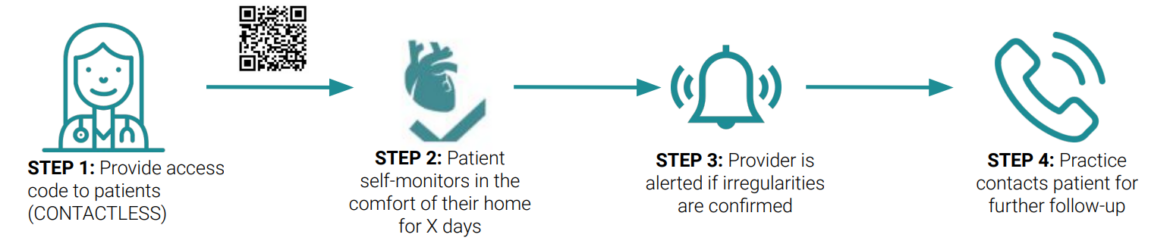
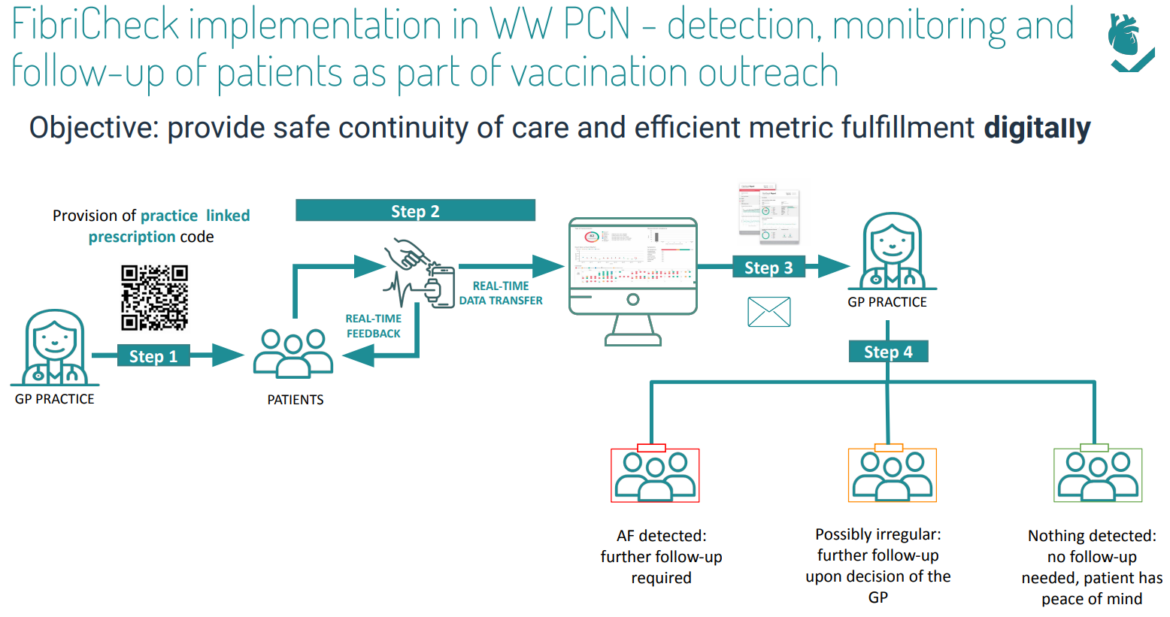
The FibriCheck flow is as follows:
Dr Shabana Ali, GP Principal at Southdene Surgery in Redbridge and Digital Lead for Barking Havering Redbridge (BHR) integrated care partnership (ICP), engaged FibriCheck through the BHR long term conditions task force, rapidly co-creating a digital case-finding approach based on the clinical Standard Operating Procedures (SOP) of Telecheck-AF, currently adopted in Barts.
The CCG selected FibriCheck based on evidence that multiple spot checks over the course of a week effectively tripled AF detection rates, which is especially critical in the early stages when episodes are intermittent and timely intervention can be lifesaving.
FibriCheck was operational in just one weekend. By leveraging practices’ flu clinic outreach to identify and engage at-risk CVD patients and including an access code on a leaflet, patients coming in for flu jabs also benefited from an AF check. All without adding additional burden to staff during vaccine delivery.
In replacing traditional in-practice pulse checks with remote FibriCheck monitoring, GP practices were able to efficiently and safely deliver distanced care, engage and improve access for hard-to-reach and shielding patients, as well as supporting stroke prevention and improved detection rates.
Impact
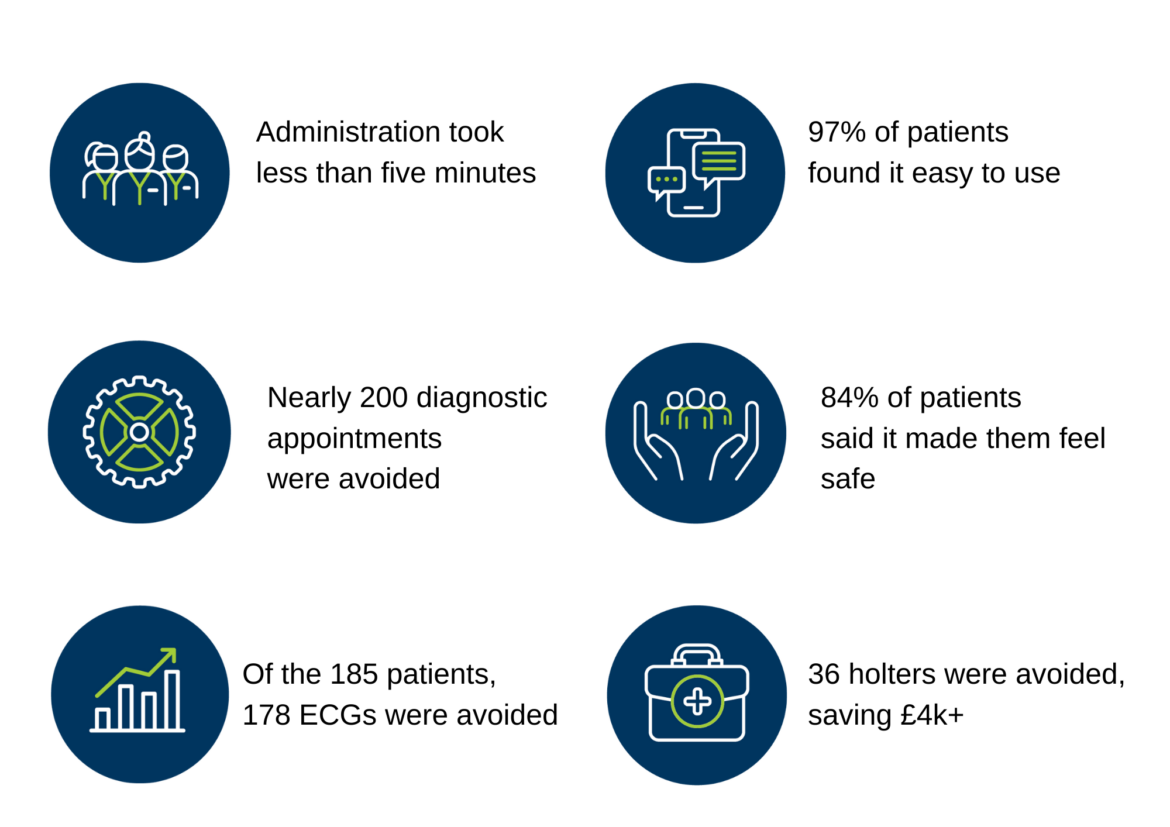
Over the six-month deployment, qualitative and quantitative data was gathered through the technology, surveys, group feedback sessions and interviews with service users, including practice staff, clinicians, managers and GPs. The findings revealed the staff overall were very positive about the technology and its value. They found it easy to onboard patients with administration taking less than five minutes per patient. All survey respondents said they would like to continue using FibriCheck and they would recommend it to their colleagues.
Patients were also positive about the app with 97% finding the installation and use of FibriCheck easy, and 86% wanting to continue using it. 84% said that monitoring from home gave them a safe feeling, knowing their doctor was informed of their heart rhythm.
Referrals to community diagnostic centres and secondary care for investigation were also avoided, showing the potential for efficiency savings in addition to reducing waitlists and backlogs. Of the 185 patients who took part in the trial, AF was found in seven patients, two of which were asymptomatic and another whom upon further investigation was diagnosed with pericarditis.
The pilot illustrated cost saving too. Most of the clinical cases who used FibriCheck would have routinely been referred for an ECG. Of the 185 patients, 178 ECGs were avoided resulting in estimated savings of £6,942. Further, a significant proportion of patients that reported palpitations where the ECG was normal would have been referred on for a 24hr holter. Taking a conservative estimate of those who reported symptoms (20%), 36 holters were avoided, with an estimated £4,356 in savings. Finally, through timely intervention of those seven patients, potential savings of £317,863 for stroke avoidance were found. Aside from savings, nearly 200 diagnostic appointments were never added to the waitlist, releasing system resource capacity for those with higher acuity needs.
Being able to reach out to patients through FibriCheck helped to empower me and my colleagues during an extremely challenging lockdown. We were able to reassure patients with normal results and alleviate their anxieties, which had been augmented due to the pandemic. It also helped to identify patients that required intervention quickly, which helps clinicians prioritise appropriate health needs. FibriCheck is easy to implement and reduces inappropriate referrals that, without this technology, could end up being a burden on the stretched health economy.
Dr Shabana Ali, GP Principal at Southdene Surgery in Redbridge and Digital Lead for Barking Havering Redbridge (BHR) integrated care partnership (ICP)
Shared Learnings
- Offering a data-driven, remote monitoring solution increased the practices’ ability to detect AF and make evidence-informed clinical decisions. The most value was in triaging symptom presentations of unknown/ at-risk patients and informing who should receive an ECG
- While the plug n’ play nature of the solution enabled rapid implementation, sustained adoption should consider integration with the patient record, as this would automate the process further and bring increased efficiencies
- Bottom-up engagement and understanding is as important as top-down buy-in. It’s important to ensure all staff groups engage in the process and that the staff involved in the front-line delivery of the service receive the training first-hand
- Implementing a new way of working always takes time to become routine practice. It is important to account for the diversity in adoption speeds, especially in multi-site deployment. Building in a change management buffer when scoping the timelines for a project will allow sufficient time to calibrate existing ways of working and fine tune new processes
- Owing to FibriCheck’s longer monitoring duration, longitudinal data triggered a change in treatment strategy of patients, supporting integrated care and shared decision making for the next steps in the patient’s journey.
AF increases risk of stroke by a factor of five and an AF stroke is much more likely to cause death or serious disability than a non-AF stroke. Treatment is highly effective at preventing AF strokes – the challenge is in getting accurate timely diagnosis in this often asymptomatic condition. Fibricheck is easy to use and accessible for patients and allows accurate diagnosis to be made remotely. This is a great example of innovative digital solutions helping to transform care and outcomes in the new world of primary care post COVID.
Dr Matt Kearney, Programme Director for CVD Prevention and Proactive Care, UCLPartners
Outcomes
FibriCheck is currently working with Barking, Havering and Redbridge University Hospitals NHS Trust around secondary prevention for stroke patients post-discharge. This year, they have also entered into joint working with Daiichi Sankyo, neoHealthTech and Capitol Medicare to offer an innovative, end-to-end digital approach to improve timely detection and diagnosis of AF at scale. This pathway transformation project will see the solution rolled out to four PCNs across the country offering GP practices a completely virtual pathway for AF detection.
If you would like to discuss FibriCheck, please get in touch with the Commercial and Innovation team on innovationteam@uclpartners.com