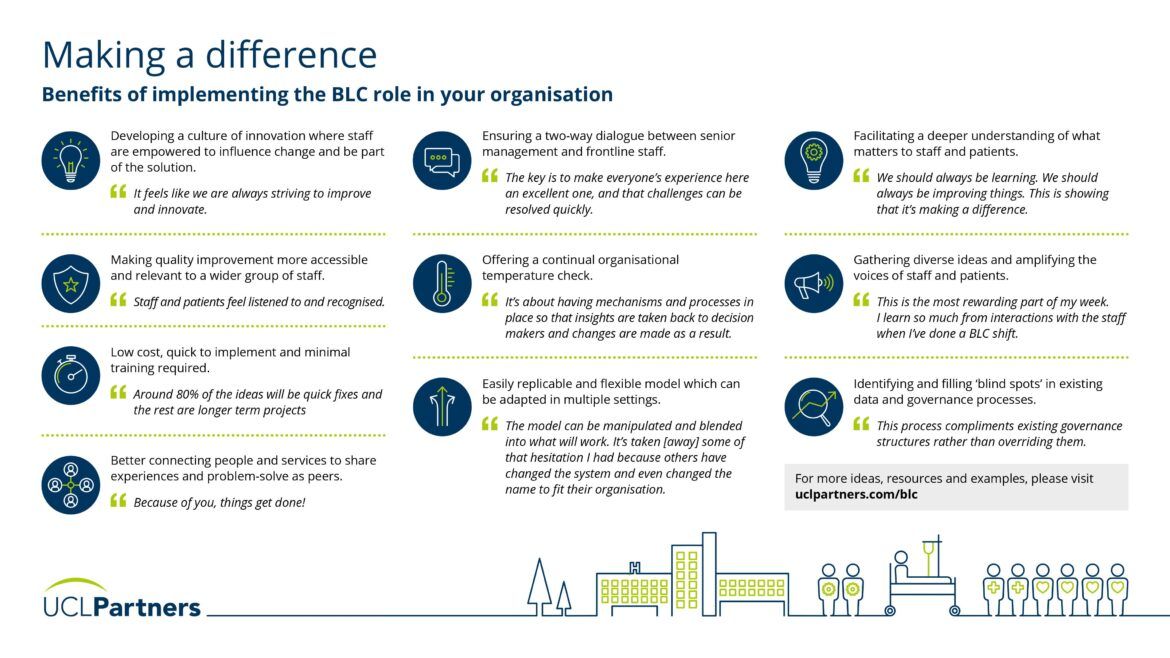
In this section, we outline the benefits an organisation can expect to see after implementing the BLC role and a learning health system approach.
The challenge
Insights from front-line staff are vital for informing quality improvement and innovation. However, health services often struggle to gather insights from staff systematically.
Front-line healthcare staff, with rich insights and ideas about how to improve patient care, workplace efficiency and staff well-being, often lack time or power to enact systemic change. In contrast, senior hospital decision-makers can effect change, but often don’t have timely access to staff and patient insights to inform changes. Insights from patients and front-line staff are rarely routinely captured and when they are, they are often underexploited.
The benefits
The Bedside Learning Coordinator role is designed to respond to this need, capturing staff insights into what is and isn’t working, supporting organisations to learn fast and act fast. The BLC role ensures frontline staff remain central to ways of providing insights and implementing changes, while simultaneously providing a mechanism to gather insights continuously without increasing burden on staff.
Strengthening a culture of innovation, amplifying the voice of staff and identifying ‘blind spots’ in existing processes are just some of the benefits identified by organisations to have implemented the role.
Additional resources:
- Three ways introducing Bedside Learning Coordinators in the NHS can improve systems and patient care: After seeing first-hand the value of the BLC role at the Nightingale, Dr Andrew Wragg shares the benefits he saw after implementing the role at Barts Health NHS Trust.
- Can a learning health system approach improve workplace wellbeing? : Dr Mike Nicholls, following a recent visit to Chase Farm, offers reflections on how to build a culture of continuous improvement, which inspires, informs, and involves staff.