UCLPartners
Impact report 2022-23
Foreword
by Dr Chris Laing, CEO of UCLPartners

This report captures a pivotal year with the launch of our five-year strategy and the start of a new way of working across our partnership.
While an exciting one, this year has seen substantial pressure across our NHS, academic and charity partners. Our health and care system is still suffering from the impact of the COVID-19 pandemic, there are backlogs, workforce challenges are considerable and the health and care system is under financial pressure.
We believe that in today’s context, the ability to work in partnership to discover and develop innovation and then deploy it at scale is more critical than ever.

This year has seen significant developments for us and our partnership. We have, following consultation, approved and launched our new strategy. Our priority themes closely align to those of our integrated care systems (ICSs), as well as to regional and national priorities. And, most importantly, they tackle what data tells us are the biggest drivers of poor health outcomes and health inequalities in our communities.
To deliver on our strategic ambitions, we have developed a new operating model that brings a specialist, integrated approach to managing a pipeline of innovation across our teams. We are working to embed a partnership approach to research, strengthening links with our university and industry partners to source innovation and supporting the building of solutions before testing them to evaluate implementation needs and their real-world impact.
Our work is guided by the health needs of our population, which is one of the reasons why we have spent this past year developing a new insights platform.

We will be working with patients, the public and our health and care system to define problems that need life-changing innovative solutions. We are ensuring that our expertise, effort and energy is spent on work that will deliver the biggest impact.
As we move forwards we are implementing our patient and public involvement and engagement strategy and working ever more closely with our ICSs, welcoming representatives from our three local ICSs and a mental health trust to our board in March 2023. A couple of months later we welcomed Dominic Dodd as our new chair and expressed our gratitude to Richard Murley for his outstanding chairmanship during a period of significant change.
We’d like to thank everyone who has worked with us this year. Together, we will direct focus onto the things that matter most and deliver on our ambitions to positively change the lives of people who need help most.
Our purpose
We are a health innovation partnership.
Our mission is to help five million people from North London to the Essex coast live longer, healthier lives.
We focus on the biggest health challenges our diverse communities are facing, prioritising the people most in need.
We solve health problems through research and innovation and speed up the delivery of solutions that improve health and care.
Our year in numbers
607 primary care networks
across England using our Proactive Care Frameworks, benefiting thousands of patients nationally
£2.1million
of funding secured to implement and test our new CVDACTION resource across eight integrated care system locations.
1,000 children and young people
have contributed their views to shape our mental health programmes.
13 NHS trusts
and 6 academic institutions participating in our climate collaborative work.
205 companies
supported to develop, test or spread their healthcare innovations this year.
39 ‘Innovations for Healthcare Inequalities’
projects started, aiming to improve access to the latest health technologies and medicines, nationally.
Developing our health innovation capability
Creating London’s Secure Data Environment
More than £13.5 million has been awarded to teams across the UK to develop a country-wide network of NHS-owned Secure Data Environments (SDEs).
Once available, the London SDE, which has so far received £3.6 million for 2022/23 and has secured a further two years of funding (details to be announced) will provide approved users (such as researchers and analysts) secure access to anonymised health and social care data for the capital’s population of more than 10 million people. Using data in this way will speed up research outcomes, meaning Londoners receive innovative care sooner.
Extensive patient and public engagement across diverse Londoner communities, including three in-depth public deliberative sessions to understand what different people think about sharing health and care information, laid the foundation for London’s SDE.
We are proud to have co-led the successful application for the London SDE programme and we will continue to work closely with patients and the public to inform decisions throughout the further development of the SDE.
The development of our insights platform

Recognising the health service collects huge amounts of data, but that more can be done to translate it into actionable insights, we have developed an insights platform that will enable us to better assess, understand and deliver against the health and healthcare needs of our diverse population.
The platform brings together publicly available health and deprivation data across three ICSs – North Central London, North East London and Mid & South Essex. Together, it paints a picture of the health and wellbeing of five million people living from North London to the Essex coast, with a particular focus on our strategic priorities.
For example, through the platform we have seen that almost 20% of people across our region have a main language other than English, most commonly Bengali, Polish, Turkish or Urdu. Also, a fifth of our communities are considered to reside within the lowest deprivation quintile, but the variation between boroughs is significant with 0% of Maldon, but 54% in Barking and Dagenham defined as such. These insights impact how we consider health inequalities in our work.
More than 50 stakeholders helped us to develop and shape the insights platform. It has three purposes:
1. Provide an easy, accessible route to understand population data for our three ICSs, enabling our health and care partners, and indeed anyone who is interested, to ascertain what health challenges the people living in our communities are facing and needing help with.
2. Create an engaging tool to publicly monitor and measure the impact of our work to solve major health challenges through our new five-year strategy.
3. Provide a means to share and contribute learning within our communities.
“North Central London ICS welcomes this new platform which will enrich the insights that we can use to tackle our biggest health challenges from a strong evidence base.”
Sarah Mansuralli, Chief Development and Population Health Officer, North Central London Integrated Care Board.
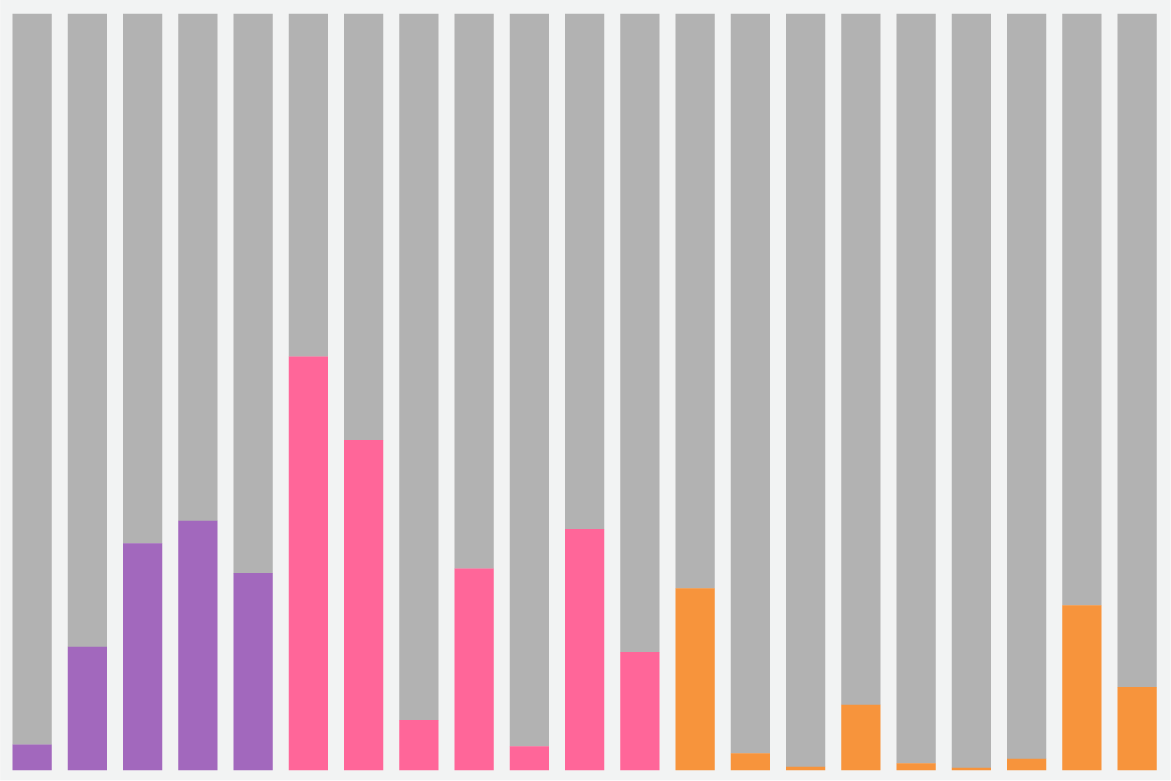
Our innovation pipeline
Insights
We will monitor our population health data to understand which of our communities are most in need. Healthcare demand and operational data will surface patient and workforce insights for impact.
Discovery
Through our academic partner relationships we will effectively track the pipeline of research and translation against our priority areas, identify promising solutions as early as possible.
Solutions
We will develop and assess promising innovations for their readiness for piloting. We will support prototype development, testing, legal compliance, market-readiness and routes to procurement.
Implementation
We will pilot innovations and scale adoption across our three ICSs, using a range of improvement and implementation science tools, and customising our approach according to local needs and feedback.
Evaluation
We are developing our real-world evaluation capabilities to enable the best support for evaluations at pilot, scale-up and national adoption levels.
Our partnership’s strength in life sciences

In the autumn of 2022, the National Institute for Health and Care Research (NIHR) awarded nearly £166m to the four NIHR Biomedical Research Centres (BRCs) in our partnership. These BRCs, part of our Academic Health Science Centre (AHSC), bring together world-leading expertise to focus on the most pressing health challenges for our population.
Some of their highlights this year include:
NIHR University College London Hospitals BRC identified a new type of MRI scan called VERDICT MRI that can help doctors diagnose prostate cancer more accurately and reduce the number of unnecessary biopsies by 90%.
NIHR Moorfields BRC launched an experimental high-volume diagnostic centre, HERCULES, which targets patients who face lengthy treatment delays and further disease complications. It is estimated that HERCULES could aid detection of 1,100 patients at risk of loss of vision per year.
NIHR Barts BRC established itself as a global reference centre for a new ‘Jenavalve’ technology. This was after successfully treating 15 patients in England with the valve implant that is specifically designed for people living with unmanageable aortic regurgitation.
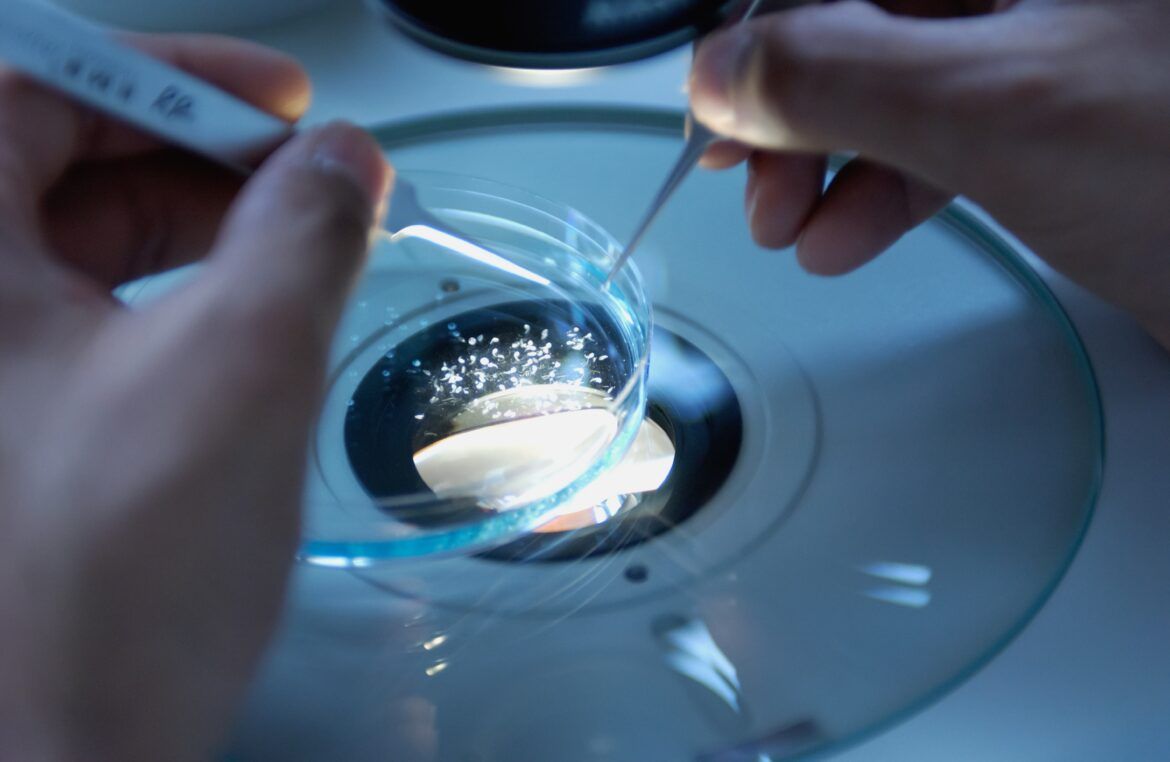
NIHR Great Ormond Street BRC started a new industry collaboration to design and develop a delivery system for photoreceptor cell patch implants that could enable retinas that are damaged to regenerate, improving a person’s vision.
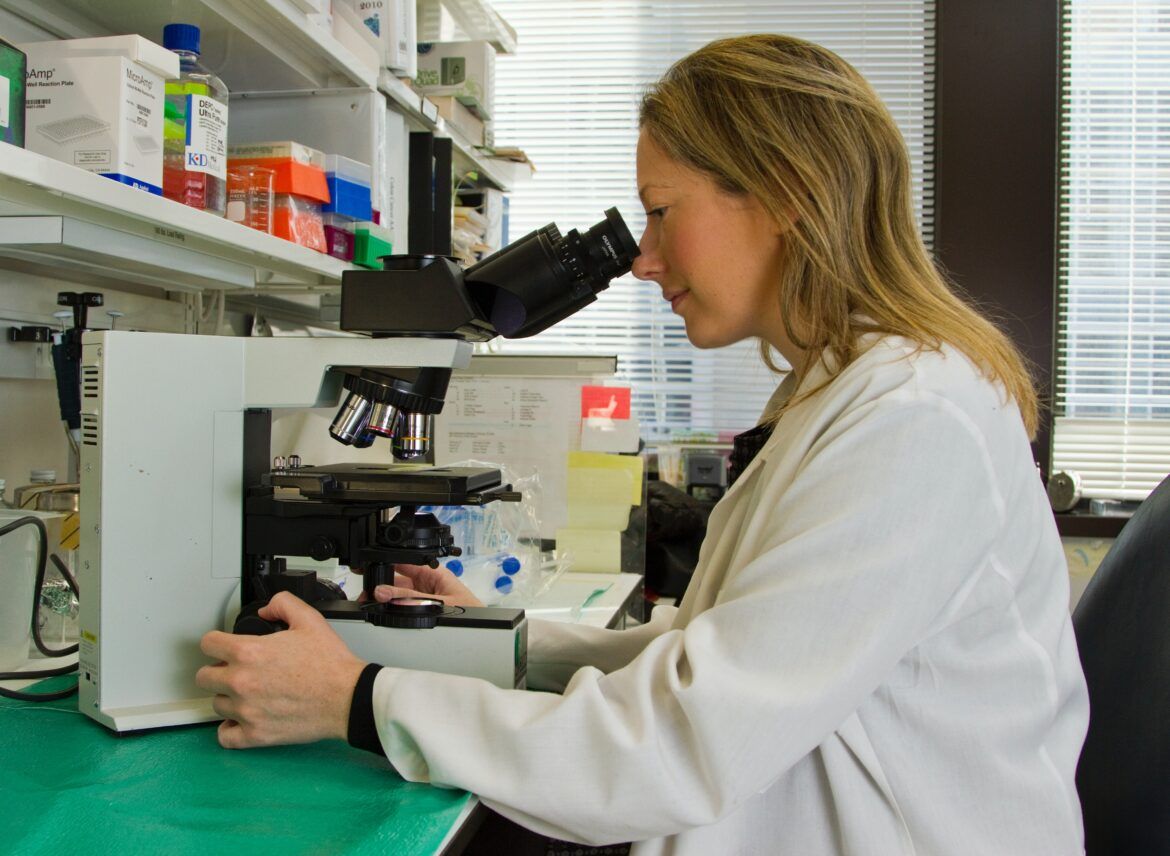
How we have supported industry

We work closely with industry and innovators to provide bespoke advice on how they can work with the NHS to test and scale their innovations. By supporting our partners to develop new relationships with industry, we help patients access the latest evidence-based care.
Our team of experts seek to future-proof the solutions we find. This year, we have assessed the initial needs of more than 205 companies and innovators before then working alongside some to design and initiate new projects or pilots.

Some examples of our work this year include supporting the adoption of 78 FeNO devices across our geography. Achieving this has helped provide more patients with a non-invasive method of testing for asthma. To date, close to 39,000 diagnostic tests have been carried out.
We have also begun a feasibility assessment of qXR, an artificial intelligence (AI) testing tool. Our work will show whether the tool is able to improve diagnostic efficiency and therefore aid earlier detection of lung cancer.
And we have been supporting Abtrace and Huma, which aim to optimise treatment of cardiovascular disease and Tiny Medical Apps, which seeks to improve management of asthma in young people. These three projects received funding from the SBRI, an Accelerated Access Collaborative initiative that in partnership with the AHSN Network awarded £6million to 14 late-stage innovations that help detect, prevent and manage cardiovascular and respiratory disease.

Alongside our direct support, we host the NHS Innovation Accelerator (NIA), an NHS-funded national programme, delivered in partnership with the 15 AHSNs, that supports exceptional individuals to grow their business while scaling promising innovations across England’s NHS for greater patient, population and staff benefit.
This year, the NIA welcomed 17 new Fellows, all of whom have created innovations that offer solutions to some of the most pressing NHS needs. Their innovations range from digital apps that can overcome language barriers and reduce health inequalities, to an artificially intelligent chatbot that can offer responsive, instant access to mental health support.

The NIA is committed to sharing learning about innovation adoption and spread with the wider health and care system. It has raised more than £200million in external funding to support patient outcomes and its fellows have won close to 200 awards for their innovations.
To date, the NIA has supported the scaling of close to 100 innovations spread across 2,882 locations of England’s NHS. This has created 1,102 new jobs. Close to 60 NIA-supported innovations have been successfully marketed internationally.
Health innovation challenges
Cardiovascular health

Cardiovascular disease (CVD) is the most common cause of death in our population and across the UK.
We have developed a suite of resources to help healthcare teams tackle conditions that increase a person’s risk of developing CVD.
One of these resources, our Proactive Care Frameworks, is enabling primary care teams to prioritise care for their highest risk patients and utilise the breadth of their workforce. This year, we have increased the adoption of our frameworks through delivery of the national blood pressure optimisation programme. The framework search tools have been downloaded 16,000 times and incorporated into the Ardens clinical decision support solution. Currently, more than 600 primary care networks (PCNs) are using our frameworks, benefiting thousands of patients across the country.
As a local example, 113 practices across Barking, Havering and Redbridge have started to use our proactive care framework that seeks to boost the management of atrial fibrillation as a CVD risk factor. As a result of this, 314 patients have started to receive anticoagulants and 2,609 patients have been identified for statins.

We are building upon the success of our award-winning frameworks with a new CVDACTION resource, which we have developed to complement the widely adopted CVDPREVENT tool.
CVDPREVENT utilises routinely held GP data to help primary care teams understand how many people with CVD, or risk of CVD, are potentially undiagnosed or sub-optimally treated within their geography. CVDACTION enables GP practices to act on CVDPREVENT data by identifying the individual patients at highest risk.

We are implementing and evaluating CVDACTION across all five London ICSs. A further three pilots are taking place outside of London; NHS England will support two of these sites and we will support one in Mid and South Essex. Evaluation of impact is expected in late 2024.

We have also continued our work to support getting patients with high cholesterol onto medications that are proven to reduce their risk of CVD. This year, 143,928 patients have been prescribed Ezetimibe and 458 have been put onto PCSK9i as a result of our work.
“The work done in Havering North (in implementing the UCLPartners frameworks) has had real impact on not only the patients, many of whom have had their hypertension brought under control, but also the colleagues across the PCN who have found this new way of working incredibly valuable.”
Dr Ann Baldwin, programme lead for five PCNs across Barking, Havering and Redbridge and Havering North PCN clinical lead
Adolescent mental health
An estimated 75% of all mental health problems are diagnosed by the age of 25, with those living in more deprived areas at higher risk.
Developmental science shows young people need agency to enjoy good mental health. This is why we are working with our partners to create a prevention-focused framework that puts co-production at the heart of policy design for children’s mental health services.
This year, we have taken on the lead delivery role for Kailo in Newham. Funded by UK Prevention Research Partnership, we are engaging with young people, their friends and families to develop a series of co-designed strategies that address the most significant systemic drivers of adolescent mental illness in the borough.

We are also working with Havering council to roll out #BeeWell. Designed by young people, #BeeWell surveys the wellbeing of pupils in secondary schools, providing insights to improve and protect children’s mental health. We are supporting a census-style survey roll-out for all year 8 and year 10 children across all secondary schools in Havering, paying specific attention to the needs of children with special educational needs.
In collaboration with the National i-THRIVE partnership, we have started to assess and design an evolution of THRIVE, a nationally implemented framework that is working to create resource-efficient communities capable of supporting the mental health and wellbeing of children, young people and their families. Our aim is to incorporate evidence of the needs of children and young people in the post-pandemic world into a redesigned delivery model.
We are working to reduce restrictive practice in mental health, learning disabilities and autism inpatient services. Currently, 16 wards across four of the mental health trusts in our geography are working with us.

Finally, we have continued our work to support the adoption of the computer-based QbTest, which aims to improve the diagnosis of attention deficit hyperactivity disorder (ADHD). This year, 1,087 children have been diagnosed with ADHD through the QbTest and NICE have now published a Medical Innovation Briefing, highlighting the benefits of the testing technology.
“BeeWell has been incredible to be a part of. This is because everything was discussed thoroughly and lots of decisions were made that would be effective for young people to answer such as lifestyle, personal self-worth and many other things. I felt listened to and was always included in decisions. I really love working with the team and helping out and if I had the opportunity again I would happily get involved.”
Saffy Kelly, Havering #BeeWell youth steering group member
Climate
Climate change poses a significant threat to physical and mental health. Our NHS feels the strain of these health implications, yet it is also a key contributor to them, responsible for 4-5% of England’s carbon emissions. National targets dictate all NHS trusts must reduce their direct carbon emissions by a minimum of 80% by 2032 and achieve net zero by 2040.
This year, we launched our Climate Collaborative, working closely with our NHS partners to identify and address blockers for their net zero ambitions. Through our engagement we identified three key areas where we can support the application of research and innovation to accelerate progress toward decarbonising the NHS.
These form the pillars of our Climate Collaborative strategy and are:
1. closing the research evidence gap through closer collaboration between our university and NHS partners,
2. reducing energy demand and greening its supply,
3. building capacity and confidence to improve carbon-based decision-making and embed sustainable change in practices.

Focusing in on pillar one of our Climate Collaborative strategy, our Connecting for Change project has created more opportunities for academic and health collaboration. Through a series of ‘sandpit’ events we brought together more than 30 people with varied expertise, challenging them to work together and propose ways we could reduce carbon emissions associated with the NHS estate and the relationship between buildings and clinical pathways. From this process, we will fund a number of collaborative novel research projects that will provide actionable evidence for removing the barriers to rapid decarbonisation.
How our work is tackling health inequalities

Across our partnership, we are working together to identify, implement and evaluate innovations that will have a life-changing impact for those who are most at risk, reducing health inequalities across our communities.
This year, we have taken on the lead delivery role for NHS England’s Innovations for Healthcare Inequalities Programme (InHIP), which sees teams from across the country working with their local communities to identify, address and minimise healthcare inequalities. Currently, there are 39 active inHIP projects aiming to improve access to the latest health technologies and medicines.
We have also continued our work to roll-out UCLP-Primrose across our PCNs in Camden and Islington, Tower Hamlets, Barnet, Enfield and Haringey. UCLP-Primrose is an integrated primary care service that seeks to better predict and manage CVD risk in people living with severe mental illness (SMI). People living with SMI experience some of the worst health inequalities, with a life expectancy of up to 20 years less than the general population. It is estimated that for people with an SMI, 2 in 3 deaths are due to a physical illness such as CVD, which can be prevented.
Recognising that physical health and mental health are often intertwined, and that one can exacerbate the other, we have developed an Integrated Maturity Matrix that aims to enhance integration of mental and physical health care in acute care settings, which is currently being prepared for a pilot across NCL.

We worked with NCL Digital Care Homes to conduct a qualitative study that has enhanced understanding of how barriers to adopting Whzan Blue Box, an innovative digital solution that is proven to improve health outcomes for deteriorating care home residents, can be overcome. With these insights and with support from NHS Innovation Collaborative, we have been able to successfully scale Whzan Blue Box across 50% and 95% of care homes in NCL and MSE respectively.
We have also worked collaboratively with our Integrated Care Boards (ICBs) and regional Patient Safety Specialists to design and deliver a bespoke set of workshops to guide and enable the implementation of the new Patient Safety Incident Reporting Framework (PSIRF) across our 21 NHS provider partners.
More than 155 GP practice staff participated in our DeStress training helping them to better support patients presenting with poverty-related distress. We have also supported the NCL Diagnostics Access programme, informing the set up and development of the Wood Green Community Diagnostic Centre, to deliver on their ambitions for having a positive impact on healthcare inequalities.
A values-based partnership

We want our work to have the biggest positive impact on the health and care of our population, helping those who are most in need and reducing inequalities.
We strive to become a more diverse and inclusive organisation. Our Equity, Diversity and Inclusion (EDI) working group, formed of UCLPartners staff working across the organisation in a range of capacities, helps to steer our work to become a more inclusive and diverse organisation.

We are also committed to creating inclusive patient and public engagement opportunities for people from diverse backgrounds and experiences to share their insights and actively shape our work.
This year, we set up our Patient, Carer and Public Advisory Panel – a diverse group of 24 individuals who feed into and influence decision-making at UCLPartners. We are also growing a broader network of patients, carers and public contributors, known as the Lived Experience Network, who share their views and knowledge, working with projects from across our area to make sure that we are tackling the biggest health challenges and developing solutions that work.

Our newly formed Environmental, Social and Governance (ESG) group, brings people from across our organisation together with the united goal of setting our standards for measuring and improving our impact on society and the environment. As part of this work, we have started measuring our carbon footprint as an organisation, with the aim of establishing 2022/23 as a baseline so that we can set out a plan for reducing our carbon footprint in subsequent years.

“By working with communities we can gather in-depth information, find new voices and connect with new ideas to work together for better health services and healthier lives.”
Dele Oladeji, UCLPartners patient, carer and public panel member
Future vision
By Dr Chris Laing
Our potential as an innovation partnership is as great as the challenges our health and care system is facing.
As we move into our next phase of strategic delivery, I believe we need to remind ourselves of our purpose and values (partnership, pace, people and population).
First, we are a partnership, and by realising the potential of our diverse capability and the benefits of working together we can drive impact where it is needed most. But we must hold ourselves to account on this at a leadership level, as only then, will we systematically eliminate the barriers we face (technical, cultural or financial) to working collectively.
Second, we need to move at pace and be ambitious with our timelines. The problems we’re facing today are not insurmountable, but they are urgent; delaying action cannot be an option.
Third, we must ensure patients and the public are integral to the development and deployment of our solutions. The answers we find must be applicable to real-world settings and scenarios, they cannot merely work in theory.
And finally, we need to ensure that we continue to focus on the largest health and care challenges that face our 5.3million population, remaining authentic in our prioritisation of the most disadvantaged groups.
It is easier to state these values than to realise them, but that is our challenge and it is something I am committed to.
I believe our new operating model will help us to work with partners, industry and the public in the most beneficial way possible and that we have the focus across our partnership to identify the innovative solutions that have the best chance of succeeding.
So, I am approaching the forthcoming year with a great deal of excitement and optimism, but also a clear understanding of the responsibilities we shoulder.