Foreword
Dr Chris Laing, CEO

We are an innovation partnership. Our job is to deliver novel solutions to challenges in health and care.
We believe innovation is a process not a product. We want to be good at making it happen. This means taking a problem, inventing or sourcing a solution, developing it, testing it, scaling it and evaluating it. If it works, we want to ensure the benefits will be sustainable.
We work with health and care providers, universities and industry. We try to work on problems that are difficult and may require a step change in how we do things to make progress. In doing so we want to improve healthcare and reduce health inequalities.
Last year we started implementing our strategy. We are making progress but there is a lot more to do. This report sets out some of the things we’ve done in the last year. Next year we would like to do more.
I’m proud of what my team and our partners have achieved in the last year and I’d like to thank them for their hard work.
Our year in numbers
£25m
938
225
800k
1.8m
How we work
Over the last year we have been developing our approach to innovation. It’s a team sport and involves people from across our specialist functions and our partners. We use our method to develop a pipeline of solutions and implement them. We are improving this over time and starting to see impact.
Our innovation pipeline
Insights
Gather insights from patients, professionals and researchers, locally and across the world.
Discovery
Understand the context, what the need is and what we know from research.
Solutions
Test ideas, models and prototypes quickly and safely to build solutions.
Implementation
Deliver solutions at scale, in partnership with systems and providers.
Evaluation
Gather evidence to quantify, prove and understand our impact.
Our priorities
We have chosen some priority disease areas. These are some of the big health challenges of our time. They drive mortality and poor health in our population and more widely. We also work on the design of health systems and we are working to make healthcare more sustainable.
Clinical priorities
Adolescent mental health
Most mental health problems develop by age 25. Rates of mental health problems are rising. People living in deprived communities are most at risk.
We have been working with our partners and communities on some solutions that we hope will help. We aim to prevent mental distress in young people and when it happens reduce harm from it.
Improving our understanding of young people’s mental health
Problem:

How do we get data to improve our understanding of young people’s mental health needs so we can support them?
Solution:
We worked with Havering Council on a solution to help them understand the mental health needs of young people in their schools. We adapted the #BeeWell survey to get data on what was important to young people in Havering. This was collated, digitised and made available in accessible dashboards. We worked hard on data visualisation to ensure this information was accessible and easy to action. The council called this survey the ‘Havering Youth Wellbeing Census’.
We supported 10 schools and 2,287 students across years 8, 9 and 10 to take part. We are now supporting the schools to develop action plans. The findings are now publicly available, and have been shared with young people’s service across Havering. The council will now be able to run the survey in future years.
“Many don’t like to say to teachers and friends that they aren’t ok at the moment. So I think it’s really good that the school got people to take the test”.
Emilie, student at Sanders Draper School
We hope this solution will help the council and local community to improve the experiences of young people, such as the students of Sanders Draper School. You can hear what they thought about this project in this video below.
“The outcome isn’t just the data, it’s the relationship and what we make of it going forward.”
Mark Ansell, Director of Public Health, Havering Council
Engaging young people in mental health to help meet their needs

Problem
How do we get young people involved in mental health prevention so they can ensure interventions meet their needs?
Solution
We are working on Kailo with communities in Newham. The Kailo solution is a platform, or method, to understand drivers of poor mental health in young people and address them. It takes a structured approach to a discovery phase, where drivers of mental ill-health are identified. This is followed by a design phase that results in interventions or policies to improve mental wellbeing in a way that is specific to locations and communities. Young people participate throughout.
In the last year we worked with 5 community partner organisations and 38 young people across Newham. One group of 14-17 year olds identified a gap in access to community support facilities and networks. A group of 17-25 year olds identified violence and crime as drivers of psychological stress. Since then we have worked with them and community partners on ways to address these problems.
We believe Kailo may be a scaleable solution to support adolescent mental health prevention across other communities and geographies. We are working with Kailo partners in North Devon to compare results.
We’d like to recognise CareCity and the North Thames Applied Research Collaborative who have helped with this work.
Improving self-referral to mental health services

Problem
How can we make self-referral to mental health services more accessible and effective?
Solution
Mental health services across the NHS are facing a lot of strain. We have seen a 21% rise in referrals for NHS Talking Therapies over the past two years.
Limbic Access has been developed by Limbic. It is an AI-enabled, self-referral clinical assessment solution. It serves as a digital gateway for patients, guiding them through the referral process on the Therapy For You website. Essex Partnership University NHS Trust (EPUT) has implemented this solution to improve the efficiency and effectiveness of the referral process. We have been working with them to support this. Previously EPUT’s self-referral process relied on patients calling the service during office hours. Minimal clinical data was collected. Limbic Access has transformed this process by allowing patients to self-refer anytime. Comprehensive data is now collected to aid these clinical referrals.
Patients using the tool were 45% less likely to drop out and more than twice as likely to complete a clinical assessment. Additionally, 37% of referrals were made outside of working hours. This showed the flexibility of the system.
Cardiovascular health
Cardiovascular disease (CVD) is one of the biggest causes of death in the UK. It also causes inequalities in life expectancy and healthy life expectancy. The good news is that there are effective and readily available treatments. These can rapidly reduce the risk of heart attack and stroke through optimising blood pressure and blood lipids. The bad news is that hundreds of thousands of people don’t access them. This is in spite of our health service having data that shows that they need them.

Making the case for cardiovascular prevention
Problem
How do we help healthcare systems make the case for cardiovascular prevention?
Solution
We identified a need from local health system leaders to understand more about the potential of CVD prevention population programmes. We brought together data from CVDPREVENT, a national primary care audit, with local health system data. We then used this to create an analytics and data visualisation solution.
We have called this solution Size of the Prize. This demonstrates the scale of the opportunity in each healthcare system. That is, if patients were treated to target, how many cardiovascular events would be prevented, how many deaths would be avoided, and how much money the NHS would save. We then think this makes a strong case for targeted intervention.
The latest data available shows that, just for our geography, optimising blood pressure for 80% of patients would impact almost 79,000 people, save over £13 million and save over 370 lives. Getting lipid management right for 95% of people we know have CVD would impact 18,000 people and save 131 lives.
Size of the prize is now available for free to all health systems in England. It has been influential in CVD prevention being prioritised in policy, improvement programmes and innovation.
Identifying and treating patients at risk of CVD

Problem
How do we identify patients who have treatable cardiovascular risk and then ensure they get effective treatment?
Solution
We identified a need from healthcare systems in London and the NHS London Regional team for a solution to identify patients at risk of heart attack and stroke.
We developed a smart-data tool that identifies patients who have one or more of six high-risk conditions for CVD: atrial fibrillation, high blood pressure, high cholesterol, chronic kidney disease, pre-diabetes and diabetes.
The tool uses data routinely gathered in primary care health records. It integrates the results of around 85 searches into user friendly, accessible dashboards. GPs can look at these and then access embedded resources to support clinical management. Searches targeting ethnicity, socioeconomic groups or vulnerable groups such as those with serious mental illness or learning disability can be undertaken. This makes this a practical way to address inequalities rapidly and at scale.
We have called this solution CVDACTION.
With funding and support from the NHS London regional team CVDACTION is being implemented across 81 practices in 10 primary care networks within London and 4 in Mid and South Essex. Our team is supporting each of the pilot sites, which cover around 800,000 patients. We are also undertaking a real-world evaluation of impact.
So what is CVDACTION telling us? Baseline data, just from patients already onboarded, identified 600 patients with dangerously high blood pressure. Another 3,300 were not treated to target. More than 5,000 patients with CVD are not on any lipid lowering therapy like a statin and nearly 18,000 are not on the right dose.
More than 1800 patients have been contacted since sites started using CVDACTION and more are being contacted every week.
Read more about our early insights into how its going, while some early adopters have shared what they have found.
We look forward to sharing our evaluation of the impact of CVDACTION with you in due course.
“By using CVDACTION we are trying to proactively prevent CVD, which might not have otherwise been done. The tool provides a helpful way to pick out patients who need care early on and offers a safety net for looking after patients.”
Romil Mandvia, Pharmacist & Cardiovascular Disease Lead
Creating a network of primary care clinicians to lead CVD prevention
Problem
How do we support primary care clinicians to lead cardiovascular prevention transformation programmes?
Solution
Our local health systems identified a need to develop a network of clinicians who can deliver impact in CVD prevention.
We developed a programme that we have called CVD Academy. Aimed at GPs, pharmacists and nurses working in primary care, the Academy supports these clinicians to implement their own cardiovascular transformation projects.
Twenty-four clinicians from across our region have joined the programme: meet the cohort.
“I joined the CVD Academy to share my ideas and learn from others.”
Bilal Mukhtar, Pharmacist
Early cancer

Cancer, when you bring together all-types, remains the commonest cause of death in the UK. We know that early detection of cancer is key to improved outcomes. This is why early cancer detection is a key priority of the NHS and one of our innovation priorities. We also know that receiving a cancer diagnosis can have a huge impact. It destabilises lives and compromises people’s ability to stay on track with treatment. Finally, we know this diagnosis falls hardest in those whose circumstances are most difficult.
Supporting patients through their early cancer journey
Problem
How do we adequately support people with a new cancer diagnosis and ensure they stay on track with treatment?
Solution
We were approached by Macmillan Cancer Support who were interested in implementing the Improving Cancer Journeys (ICJ) intervention in England. ICJ was developed in Scotland. With this approach financial, emotional or other practical support is tailored around the individual. This is designed to make their early cancer journey easier and keep them in treatment. We call this holistic support.
Macmillan research has shown that having cancer costs a household an average of £891 per month. This is from lost income and increased costs such as travel and childcare. In 2020/2021 there were 16,861 new cases of cancer reported across our area. 48% of these waited more than two months for their first treatment after their diagnosis.
We made a video outlining the experience of people with a new cancer diagnosis – view this below.
We are using our innovation skills to work with local health and care partners and Macmillan to improve holistic support in the early cancer journey.
In the last year we started working with three sites: Enfield and Haringey, Barking and Dagenham and Southend. We picked these sites as we knew, from looking at our data, they had the biggest inequalities in early cancer.
We are mapping out the patient journey at each hospital, understanding what support and services are currently available to patients and their families. We are also reviewing available data to create baseline measures. We are then getting insights from the local community. We will then support the design and delivery of early cancer support that works best for those who are most deprived.
This is the beginning of a four-year journey. We are looking forward to working with partners in health and social care as well as voluntary and community sectors to take this work forwards.
Improving cancer treatment with predictive modelling

Problem
How can we predict liver and kidney damage from cancer chemotherapy so we can mitigate harm?
Solution
28% of all patients with a cancer diagnosis need chemotherapy treatment. While a proven option, there are risks. Kidney and liver damage can be caused by some cancer drugs. So predicting and averting risk of these harmful effects could benefit a large number of cancer patients.
Evergreen Life, Durham University and University College London Hospitals NHS Foundation Trust have developed a proof-of-concept AI solution. This can accurately predict the risk of kidney and liver damage after cancer drugs.
We are leading on health economic modelling, patient and public involvement and stakeholder engagement. With this support we hope we can help can take the design of this solution to the next stages.
Patient safety

We are commissioned by NHS improvement as a health innovation network to lead a local patient safety collaborative. In this programme healthcare providers and commissioners collaborate across our footprint in North Central London, North East London and Mid and South Essex. We are working to achieve the objectives set out in the NHS Patient Safety Strategy through implementing the National Patient Safety Improvement Programme.
This year the programme has prioritised systems, managing deterioration, medicines, mental health, and maternity and neonatal safety.
We have worked with maternity and neonatal units across our region to improve the outcomes for mothers during pregnancy. We also want to ensure preterm babies get the best start in life. This includes support for the implementation of the Preterm Perinatal Optimisation Care Pathway. Our work here had the following impact:
- We helped 938 women giving birth at less than 30 weeks of gestation to receive magnesium sulphate within the 24 hours prior to birth. This means, according to NHS England estimates, 25 babies will not develop cerebral palsy. As well as the avoidance of such long-term harm to individuals this will save the health and care system between £20 million and £25 million.
- We supported survival of between 41 and 62 babies, born at less than 34 weeks gestational age, who had their umbilical cord clamped at one minute after birth.
- We supported 353 women in preterm labour at less than 34 weeks of gestation to receive intravenous intrapartum antibiotic prophylaxis to prevent early onset neonatal Group B Streptococcal infection. This potentially means that 35 babies were born without Group B Strep and that eight babies survived due to this intervention.
- We estimate between 14 and 18 lives were saved because the mother was administered antenatal corticosteroids.

We also worked with our integrated care boards and regional Patient Safety Specialists to support safety improvements across the system.
Finally, we worked with healthcare professionals across 21 NHS provider partners to implement the new Patient Safety Incident Reporting Framework (PSIRF) through a series of workshops and peer support sessions. All the healthcare providers successfully transitioned to the new system by end of March 2024.
Respiratory health
The UK has the worst asthma mortality rates in Europe for the 10-24 age range. We also have one of the highest emergency admissions rates (Nuffield Trust and RCPCH data). One million children and young people in the UK are living with asthma. Fewer than 25% have a personalised asthma action plan in place.
Improving asthma control for children and young people

Problem
How can we improve asthma control for children and young people through improved self-management?
Solution
Tiny Medical Apps have developed a Digital Health Passport. It is an asthma and allergy self-management application designed for teenagers, young adults and the patients and carers of children. It’s been designed to make patient-facing aspects of the care pathway smart and effective.
We were asked to independently assess the impact, effectiveness and value of this solution. We designed the evaluation then used mixed-methods data collection to provide a holistic and robust data set. We then analysed qualitative and quantitative data, including health economic analysis.
Our evaluation identified clear, statistically significant evidence of improvement in patient activation and asthma control.
Through support from the Health Innovation Networks Tiny Medical Apps have secured over £0.5 million in business.
“UCLPartners have been excellent evaluation partners. Their insight will help our NHS clients overcome barriers to scale and effectively get the Digital Health Passport to underserved populations where it is needed most.”
Greg Birch, Tiny Medical Apps Founder and Medical Director
Vision
Eye problems are the commonest cause of outpatient appointments in the NHS. Visual loss is a leading cause of chronic disability and the burden of blindness falls hardest on those from deprived communities. One of our partners, Moorfields Eye Hospital, is a global leader in eye health and oversees the only eye care biomedical research centre in the UK.
Evaluating improvements to the eye referral pathway

Problem
How do we transform the eyecare pathway to streamline access, reduce waiting times, improve outcomes and reduce cost?
Solution
We were approached by Moorfields to act as an innovation partners for their eyecare pathway transformation work. Key components of their pathway are a single point of access for all eye-related referrals and initial assessment in community based diagnostic hubs. Through a strategic partnership we are doing cross-pipeline innovation support to help them develop and scale this care model.
Initially we were asked to help evaluate the existing pathway and model its impact if scaled up. We did an evidence review and cost consequence analysis of the single point of access intervention. We also created a demand and capacity model for their proposed diagnostic-hub based pathway. We have been able to demonstrate to Moorfields the impact of their work. This is in patient experience of waiting times and travel distance, optimisation of the referral journey, cost savings to primary and secondary care, contribution to net zero and rapid triage of urgent referrals.
Our modelling has since contributed to national development work on the future of eyecare. We continue to work closely with Moorfields to model and forecast the impact of a wide range of solutions on outcomes and experience for eye care in London.
Transforming dementia care
If you unbundle cancer into subtypes, dementia is the leading cause of the death in the UK. We know that 27,000 people in our region have dementia and we estimate an additional 15,000 people have dementia that has not been diagnosed. Alzheimer’s Research UK estimate that dementia will be the costliest health condition in the UK by 2030. Dementia cost the UK £25 billion in 2021 and this cost will rise to £47 billion in 2050. Currently, 1.1 billion hours per year are spent on unpaid care for dementia patients in the UK.
Improving the dementia care pathway
Problem
How do we transform the dementia care pathway to improve diagnosis, care and access to emerging diagnostic and therapeutic innovation?
Solution
We have identified a need for a new approach to dementia care in our healthcare systems. We are also aware of the strength of the discovery space. Potentially transformative diagnostics and therapeutics may be coming. We need to get ready for this future now. We are lucky to have internationally leading experts, researchers and institutes on our patch, including the hub of the UK Dementia Research institute, led by Professor Nick Fox, and the coordinating centre for the dementia translational clinical trials network, led by Professor Cath Mummery (Head of clinical trials and novel therapeutics, UCL Dementia Research Centre).
We want to ensure we have a care pathway in place that provides better baseline care and then can accommodate these breakthroughs, accelerating access to them across the population. In short, we want to build an internationally-leading system for dementia care and progress.
We are at the start of our journey here. Our senior advisors Dr Ruth Dobson (clinical senior lecturer in preventive neurology, Wolfson Institute, QMUL) and Professor Rimona Weil (UCL Dementia Research Centre) have audited memory services across our geography. They have also evaluated the likely patient-level eligibility for new, disease-modifying therapies in Alzheimer’s disease. We have also assimilated learning from the introduction of disease modifying therapies on multiple sclerosis to inform our next steps.
Hear more from Dr Dobson and Professor Weil in the video below.
Earlier this year we brought together a wide group of experts, patients, carers and stakeholders with healthcare system leadership. We wanted to learn from the latest research about new disease modifying treatments and discuss current thinking around modelling services across the disease pathway. It was an opportunity to further cultivate the relationships, discuss future collaboration and focus our efforts. The group identified inequalities in dementia care, patient and carer needs, access to disease-modifying therapies and biomarker testing as key to pathway design.
We are now teaming up with healthcare, charity, university and industry partners and planning next steps.
Creating future healthcare systems
Climate
Climate change is one of the biggest problems we are facing. The NHS and our healthcare partners have committed to achieving net zero. We want to help with innovation that makes sustainability of the healthcare system a reality.

We were approached by the NHS England green team to work with them to develop solutions that might be applied across the NHS. They wanted to use our unique position at the interface of healthcare, universities and industry to create solutions quickly. The result was a programme called ‘Connecting for Change: Funding NHS collaborations to help the NHS meet Net Zero.’
We used our sandpit method to rapidly define problems and got university experts to co-create solutions. We then, with NHS England support, funded these as projects.
Cutting unnecessary energy use in operating theatres
Problem
How do we safely reduce unnecessary energy consumption in operating theatres?

Solution
10% of the NHS carbon footprint comes from energy supplies. Operating theatres consume a large amount of this energy. Half of theatre energy is consumed by anaesthetic gas scavenging and ventilation systems. These are routinely left on for the 50% of time when the theatres are not in use.
Dr Anne Symons (healthcare architect, senior research fellow, the Bartlett School of Sustainable Construction, UCL) and Dr Jonny Groome, (consultant anaesthetist and greener theatres lead at Bart’s Health NHS Trust) are developing a technical approach that will enable theatre ventilation systems to be shut down safely when not in use. This work is being undertaken in Bart’s Health NHS Trust and University College London Hospitals NHS foundation Trust.
The team estimate, from their model, that this approach, if scaled across the NHS, would save 108,000 tonnes of CO2 and £90m per year.
You can read more about this project.
In related work, Ian Eames (Professor of Fluid Mechanics, Department of Mechanical Engineering, Faculty of Engineering Science, UCL) is working on a project to change perceptions about how operating theatre ventilation. He hopes to do this by training and educating clinical and estates staff.
“UCLPartners have struck gold here. This is not silo-based research. This is fast action, collaborative research that provides us with vital links.”
Dr Anne Symons. Bartlett School of Architecture, UCL
Decarbonising NHS estates
Problem
How do we use data to rapidly identify and model interventions that will decarbonise NHS estates?
Solution
Dr Esfand Burman (Associate Professor, UCL Institute for Environmental Design and Engineering, UCL) is using data already available in NHS building energy performance certificates. He is then using this to build a ‘performance stock model’. This will be used to simulate the effect of different interventions on reducing carbon emissions. The project is being piloted in primary care facilities and where Dr Burman’s team will look at the practicalities of these changes. If successful, the team hope this approach will be rolled our across 3,000 estates in the NHS property services portfolio. It will also be applicable to all buildings with energy performance certificates.
Problem
How do we take a systematic approach to reducing unnecessary emissions in perioperative pathways?
Solution
Catherine Borra and Rebecca Wood are research associate at Bart’s Health NHS Trust. Through this programme they have created a framework so changes in orthopaedic clinical pathways can be carbon costed. This means that carbon footprinting can be made central to service changes. This carbon costing will be embedded in orthopaedic clinical trial design and we hope this approach may be scaled more widely in the NHS.
“The support provided by UCLPartners is essential. The tools and network we have been introduced to is very valuable and form the first building block of the project.”
Catherine Borra, research associate, Bart’s Health NHS Trust
Health system design
We think to be sustainable our health service will need radically different models of care. These models of care will be digitally enabled and make ‘4Ps’ medicine central. 4Ps care is predictive, proactive, preventive and participatory. So in this priority area we are innovating in new ways of delivering care, cutting across disease areas.
Working with the community to improve access to diagnostic testing

Problem
How do we optimise the use of community diagnostic centres, ensuring they accelerate care for deprived communities?
Solution
We were approached by North Central London Integrated Care System to support the design and development of the Wood Green Community Diagnostic Centre (CDC). A key aim of this centre was to reduce inequalities in access to diagnostics. We worked with the clinical and management team. We provided help in clinical engagement, patient and public involvement, pathway mapping and design, data analysis, real-world evaluation and communications. We created a dashboard to triangulate data from multiple sources to engage GPs and improve uptake of direct GP access.
New pathways that were designed and are now being piloted. These include a rapid diagnosis pathway for non-specific symptoms, a targeted lung health checks pathway and a sarcoma pathway.
Community engagement was key and we ran focus groups with Black Caribbean, Turkish, Kurdish and Polish communities within local spaces across Haringey. Interventions to improve access included extended opening hours and a more flexible booking system.

We supported the CDC to increase diagnostic capacity for the largest causes of avoidable death in North Central London (cancer, respiratory disease and cardiovascular disease).
We then conducted a health equity audit. This showed that across all types of referrals access has increased for more deprived groups. Utilisation mapped more closely to the Haringey population. 75% of referral were from the 40% most deprived groups. Referrals from Core20PLUS5 groups has doubled since opening from 10% to 21%. Ongoing engagement is underway to keep improving this.
We would like to acknowledge Professor Steve Thornton and colleagues from QMUL in early development of the proposal for this project.
We have shared what we learned about community engagement doing this project.
“Hearing directly from the community we are here to serve has allowed Wood Green CDC to be designed in a way that serves the unique needs of its local population.”
Sacha Jarrett, Engagement and Communications Manager, Whittington Health
Streamlining the supply of medicines in the community
Problem
How do we streamline the supply of low-tech medicines in the community, reducing demands on homecare services?
Solution
We teamed up with Pfizer UK, Alliance Healthcare, University College London Hospitals NHS Foundation Trust and teams from across North Central London. Our task was to design, develop and deploy a pathway for supplying ‘low-tech’ medicines. These are medicines that do not require a specialist monitoring by a healthcare professional via community pharmacy. This helped free up homecare services so they can focus on delivering complex medicines that need specialist support.
Using artificial intelligence to predict and prevent emergency illness
Problem
How can we predict future urgent and emergency care demand and intervene proactively to improve outcomes for patients?
Solution
We identified a need from our local health systems, the NHS London regional team and national NHS stakeholders for new approaches to manage urgent and emergency care. There was particular interest in using predictive technology to intervene more proactively. In doing so we might stop patients deteriorating and needing emergency care.
We have since partnered with Health Navigator (HN) to deliver a solution. They have demonstrated that 80% of urgent and emergency care demand (defined by needing 3 or more days in hospital for emergency admission) is used by only 5% of the patients accessing hospitals. This group of patients are however high turnover and to intervene you need to do it before they decompensate. Finally, 80% of this demand is predictable at patient level, using artificial intelligence, from routine health data. It’s also predictable months in advance.
The HN solution uses hospital data and AI to predict future high demand users of emergency care. This is then used to provide a proactive telemedicine intervention. These coaches also interact with other community teams in the health system. Randomised controlled trials have shown, for eligible patients, a 30% reduction in acute care demand and, for elderly males from deprived backgrounds, a reduction in mortality.
We are working as innovation partners to North-East London and North Central London Integrated Care Systems to implement, optimise and evaluate this solution. It will be implemented cross the entire East London health system initially. We will be working closely with patient groups and ensuring the intervention is optimised for diverse London communities.
This three-year project is one of the largest AI implementations in the NHS. It has been supported by a significant investment from NHS England.
Health inequalities
Addressing the social determinants of health

Problem
How can healthcare providers practically act on the social determinants of health to improve outcomes for their patients?
Solution
Health inequalities are, in large part, the product of inequalities in the conditions in which we are born, grow, live, work and age. We call these the ‘social determinants of health’ (SDOH).
We became aware that several healthcare providers had innovated to deliver solutions that impacted on SDOH to the benefit of patients. We felt it would be helpful to our partners and the wider NHS to report this work as case studies and synthesise lessons.
Working with Sir Michael Marmot, we wrote up 4 case studies and synthesised 13 lessons. Our report provides a basis for other healthcare providers to get started in this area. It has been downloaded over 450 times since publication. We would like to thank Barts Health NHS Trust, East London NHS Foundation Trust, Great Ormond Street Hospital and Mid and South Essex Foundation Trust for sharing their work.
“Health care providers play an important role in helping to address inequalities and the projects showcased in this report show what can be achieved through ‘thinking big and starting small’.”
Sir Michael Marmott
Supporting the NHS as an anchor institution
Problem
How do we support NHS organisations to organise their efforts to become better anchor institutions?
Solution

NHS organisations have a significant impact on local people. This influence is not just on healthcare but in how they employ people, the goods and services they buy, the way the use spaces and the partnerships they develop. As such they are what we call ‘anchor institutions.’
We were approached by the team in NHS London Region to co-create something we have called the Anchor Strategy and Change Network. This provides an opportunity for NHS organisations to rapidly share what they are doing and learn from each other.
We also, in partnership with the Health Foundation, created a solution called the Anchor Measurement Toolkit. This helps organisations prioritise and measure the activities as an anchor institution, understand what’s working and what improvements need to be made. Over 40 organisations were involved in developing the toolkit and we had over 190 respondents to our survey. The toolkit is in wide use and has been downloaded 900 times since publication.
Innovation for Healthcare Inequalities Programme
Problem:

How do we address local healthcare inequalities experienced by underserved populations?
Solution:
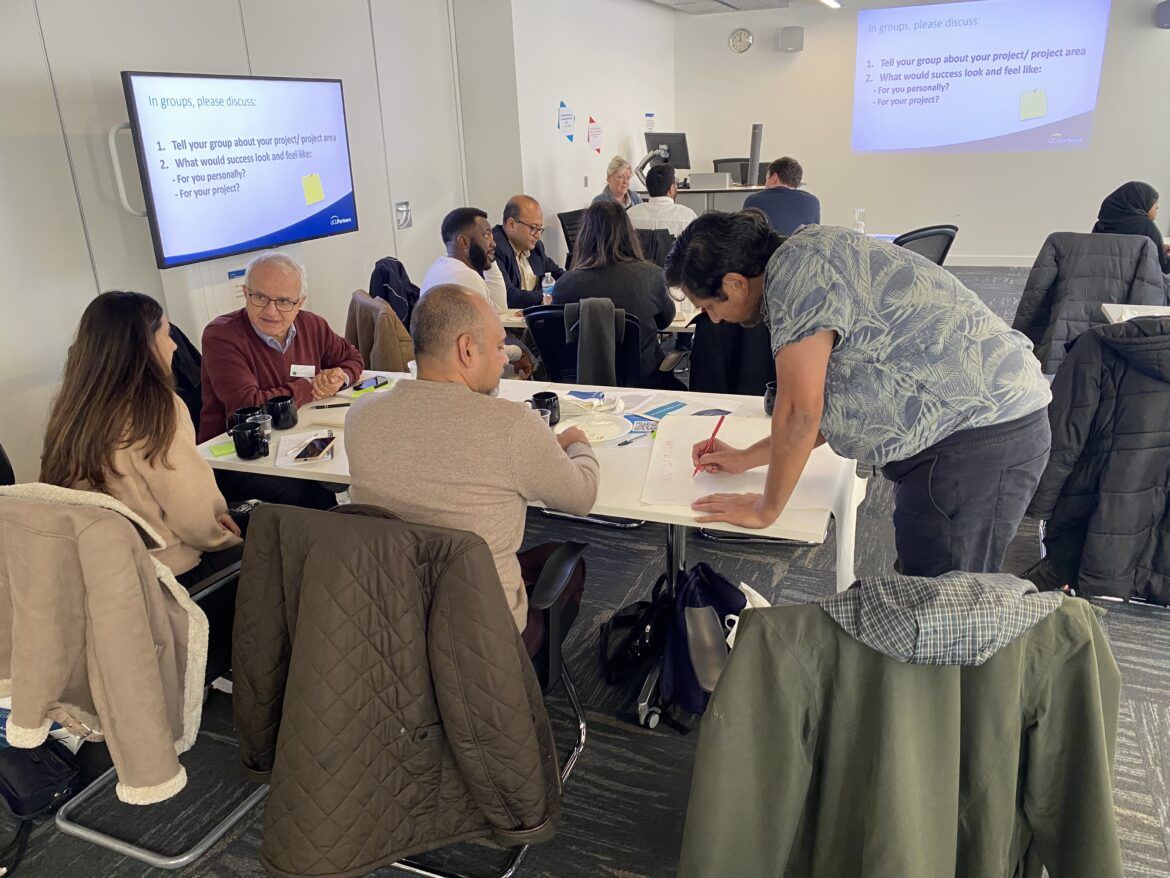
We supported NHS England’s Innovation for Healthcare Inequalities Programme (InHIP) to address local healthcare inequalities experienced by underserved populations. This was done by improving access to clinical pathways, and the latest health technologies and medicines.
Voices from local communities were essential in guiding this work to make sure that those most in need will benefit from it.
We supported project teams of clinical and non-clinical experts in our geography with data collection to inform public engagement, facilitating learning sessions, project evaluation along with implementation coaching.
As well as local implementation we have acted as a national delivery partner for NHS England on this programme. In total £4.2M was made available for innovation projects across England.
Our work with industry
We are funded by the Office of Life Sciences to support industry and innovators develop and scale their solutions in the NHS. As well as clinical benefits we want this to promote economic growth and for companies with good solutions to be successful. We have a systematic approach to this and tailor it around innovators to make sure we have most impact.

This year we have assessed the initial needs of 225 companies and innovators and worked alongside some to design and initiate new projects or pilots. This has led to innovators generating around £5.8 million in sales and/or investments.
The NHS Innovation Accelerator

UCLPartners host, lead and operationally deliver the NHS Innovation Accelerator (NIA) for the NHS England National team. We work in partnership to do this with the 14 other Health Innovation Networks.
The NIA is an NHS-funded National programme. It supports exceptional individuals to grow their business while scaling up promising solutions across the NHS in England for patient and staff benefit.
This year the programme welcomed 12 new fellows, who bring a wealth of expertise and innovative ideas to the table. These range from digital health technologies to novel care delivery models. Each fellow offers a unique solution designed to address problems in the NHS.
During the lifetime of the programme NIA fellows have gained more than £220 million in income or investment and its fellows have won over 200 awards for their solutions, spread 100 solutions across 3,271 location in the NHS, created over 1,200 jobs and successfully marketed 60 solutions internationally.

In the last year we have seen a significant upwards trajectory in programme performance metrics.
In the last year NIA fellows currently on the programme have:
- Reached over 1.8 million patients with their solutions.
- Created 106 jobs.
- Achieved over £31 million in UK revenue and over £9.5 million in investment.
- Entered 508 new NHS organisations.
- Won 38 awards.
We also developed an exciting programme to target health inequalities, working with NHS England, the NHS Race and Health Observatory and the NHS England Inequalities team.
Find out more about this work.
We would like to congratulate all our Fellows on their success and thank the other Health Innovation Networks for their support in delivering this programme.
“Through collaboration, innovation, and dedication to improving patient care, the NIA continues to shape the future of healthcare in the UK and beyond.”
Verena Stocker, interim Director of Innovation, Research, Life Sciences and Strategy, NHS England and interim CEO of the Accelerated Access Collaborative
Working towards an integrated health innovation system
Welcoming NCL Health Alliance
This year, we welcomed the NCL Health Alliance into UCLPartners under shared leadership and governance. The Alliance is the ‘all-in’ provider collaborative for North Central London. This makes us one of the most integrated health innovation systems in the UK. We are really looking forward to working with the alliance team, connecting our innovation pipeline to their service transformation projects.
The team are working on an exciting project about transforming long term condition management. We hope to share more about this in due course.
Bringing the future forwards: CASMI and IGNITE

To lead health innovation globally we need to surface the most difficult strategic challenges, identify the biggest transformation opportunities and facilitate debate and diverse opinion.
This year we welcomed The Collaboration for Sustainable Medical Innovation (CASMI) into UCLPartners. CASMI was founded by Sir John Tooke and does the following:
- Acts as a think tank for health innovation and health and care challenges
- Runs high profile IGNITE conferences, presenting and discussing the latest ideas in global health innovation
- Convenes an international network of innovation experts and collaborators, through its fellowship programme
Recent IGNITE conferences have covered health inequalities (attended by Sir Michael Marmot) and emerging biohazards (attended by Sir Jeremy Farrar).
We are currently planning future events and look forward to updating you.
Making patients and the public central to our work

We work closely with patients and the public when we design and deliver solutions. We embed our patient and public involvement and engagement (PPIE) across all our work and we pay participants for their help.
During the last year we have:
- Redesigned our Lived Experience Network
- Got 184 patients, carers and community involved in projects across UCLPartners, triple that in 2022
- Got 87 patients, carers and community members to link to our networks or governance structures
Collaborating across the Health Innovation Network
We continue to work very closely with the other 14 Health Innovation Networks on scaling up solutions nationally. We have also been working much more closely with the other networks in London on regional priorities, and also work closely with colleagues in East of England.
We’ve really enjoyed working with all of these teams and look forward to more of this in the year ahead.
Developing our early innovation offer

We would like our innovation partnership to have a clearer early innovation offer. This is in invention and early development of solutions but also in the shared infrastructure required to support it.
This year we fully integrated our early innovation/academic health science centre leadership and team into UCLPartners. We want to integrate this more fully with our later stage innovation support. We have also undertaken an external review of our early innovation pathway and this will inform next steps.
We’d like to thank our partners for participating in the review and Newmarket, led by Lord James O’Shaughnessy for undertaking it.
How we are developing responsibly as an organisation

We have now instated our environmental, social and governance group (ESG) and we are running programmes across the organisation. To show our commitment to net zero we were pleased to be the first NHS funded health innovation network to publish a carbon reduction plan.
Meanwhile we have continued our support for the HDR Black Intern Programme, aimed at enhancing opportunities for talented black health data scientists in the UK to excel in STEM careers. Read about Jessica Mtemeri and Saharla Warsame’s experience joining us as part of the programme.
Looking ahead

As we look ahead we know the health and care system is very challenged. This is causing harm, poor health and inequality. This, in turn, risks societal and economic instability.
Turning this around is going to require a lot of effort on many fronts. Innovation won’t be the whole story, but we think it’s going to have a big part, and we feel lucky to be working in this area. There are big opportunities, and we think we will have the skills and partnerships in place to make a difference. We’ve got some exciting projects we are developing that we are looking forward to sharing with you.
If you would like our help please do get in touch.